
Piecemeal cold snare polypectomy of large sessile serrated polyps is safe and effective: Cold is the new hot!
Swati Patel, MD, MS
Associate Professor, Division of Gastroenterology & Hepatology, University of Colorado Anschutz Medical Center, and Rocky Mountain Regional Veterans Affairs Medical Center, Aurora, Colorado
This article reviews Van Hattem WA, Shahidi N, Vosko S, et al. Piecemeal cold snare polypectomy versus conventional endoscopic mucosal resection for large sessile serrated lesions: a retrospective comparison across two successive periods. Gut 2021;70:1691-97. https://doi.org/10.1136/gutjnl-2020-321753
Correspondence to Swati Patel, MD, Associate Editor. Email: Evidence.Based.GI@gmail.com
Structured Abstract
Question: Is piecemeal cold shttps://webfiles.gi.org/podcastsnare polypectomy of sessile serrated lesions (SSL) ≥ 20 mm safe and effective compared to hot snare endoscopic mucosal resection?
Design: Retrospective comparison of two time period cohorts (2008-2016 versus 2016-2020) within the Australian Colonic Endoscopic Resection (ACE) Study. Setting: Four tertiary referral centers in Australia. Data from the Australian Colonic Endoscopic Resection study where patient, procedural, short- and long-term follow up data were prospectively collected.
Patients & Lesions: Lesions ≥ 2 cm with Kudo II (O) pit pattern (i.e., consistent with serrated polyp histology) were included (Figure 1). Lesions with features consistent with adenomas/dysplasia (Kudo III or IV pit pattern) or submucosal invasion (Kudo V pit pattern) were excluded from the cold snare group. 156 SSLs (median size 25 mm) treated by piecemeal cold snare polypectomy between 2016-2020 from 121 patients (median age 60 and 70.2% female) were compared to 406 SSLs (median size 25 mm) removed by standard hot snare endoscopic mucosal resection from 2008-2016 from 353 patients (median age 66 and 65.2% female).
Intervention: All lesions were examined under high-definition white light and narrow band imaging. Lesions were lifted with succinylated gelatin, 0.4% indigo carmine and 1:100,000 epinephrine. A dedicated cold snare was used to remove the lesion piecemeal ensuring a wide rim (≥3 mm) of normal mucosa at peripheral margins. Conventional hot snare endoscopic mucosal resection was performed per usual technique1 and snare-tip soft coagulation of the resection margin.
Funding: Westmead Medical Research Foundation, University of British Columbia Clinician Investigator Fellowship, Gallipoli Medical Research
Results: Piecemeal cold snare had 100% technical success per lesion, with no adverse events per patient (Table 1).
Table 1. Study Results
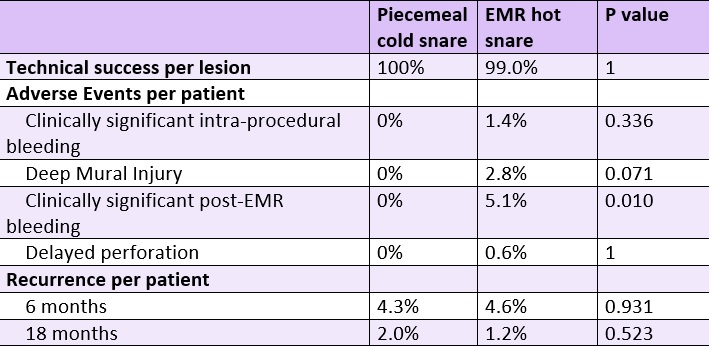
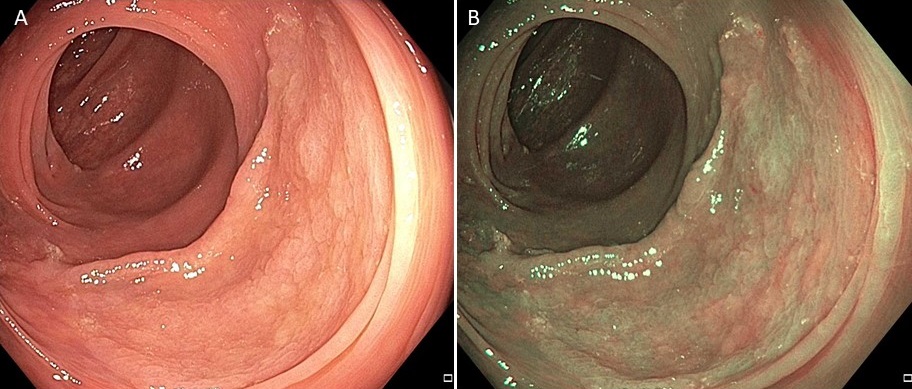
Figure 1. Large sessile serrated lesion without features of dysplasia or submucosal invasion under high-definition white light (A) and narrow band imaging (B).
Why is this important? Up to 30% of all colorectal cancers (CRCs) arise from sessile serrated lesions (SSLs) through the serrated colorectal neoplasia pathway.2 These lesions are usually located in the proximal colon, are flat, have an overlying mucous cap and have indistinct borders. Because of these endoscopic characteristics, these lesions are frequently missed,3 prone to incomplete resection4 and therefore disproportionately represent the precursor lesions to post-colonoscopy cancers.5 Thus, in addition to careful inspection during colonoscopy to minimize missed lesions, it is critically important to ensure complete endoscopic resection of SSLs.
The standard of care for removal of these lesions has been to perform endoscopic mucosal resection (EMR) with a hot snare6 and more recently to treat the resection margins with snare tip soft coagulation.7 EMR is associated with a risk of delayed post-polypectomy bleeding and deep mural injury, defined according to the Sydney classification as grade III (muscularis propria injury or ‘target sign’) or grade IV/V (transmural perforation without or with contamination, respectively).8 Given that SSLs have less submucosal fibrosis than adenomas, van Hattem et al. hypothesized that removing SSLs without submucosal invasion via piecemeal cold snare polypectomy may be just as effective as EMR. Furthermore, without electrocautery, the authors posited that the risks of delayed post-polypectomy bleeding and deep mural injury would be lower.
Key study finding: Piecemeal cold snare polypectomy had 100% technical success, similar recurrence rates (< 5% at 6 and 18 months), and 0% adverse event rate with significantly lower rate of post-EMR bleeding compared to conventional EMR, and the authors concluded that this technique should be considered standard of care for these lesions. Caution: Lesions were only removed by piecemeal cold snare polypectomy if they were SSLs and had no evidence of adenomas/dysplasia based on optical diagnosis. Furthermore, all lesions were lifted with a dye agent and epinephrine and removed using a dedicated cold snare (i.e., snare designed specifically for cold snare polypectomy). Although all lesions in this study were resected by an experienced endoscopist, widespread use of cold snare suggests that any endoscopist can adopt this approach for large serrated lesions.
My practice: I dedicate time and effort to adequately cleansing the lesion (to wash off any mucous cap) and thoroughly inspect the lesion under high-definition white light and Narrow Band Imaging (NBI) to ensure the lesion is an SSL based on Workgroup on SerrAted polypS and Polyposis (WASP) criteria9 and does not have any features of adenomas/dysplasia (Kudo III or IV pit pattern) or submucosal invasion (Kudo V pit pattern). I lift all lesions with a dye-based colloid injectate. Specifically, I use ORISE (Boston Scientific, Marlborough, MA), but Eleview (Areis Pharmaceuticals, San Diego, CA) is appropriate, too. I also use a snare designed specifically for more complex cold snare polypectomy instead of a standard oval snare. Currently, I’m using the Captivator™ COLD Single-Use Snare (Boston Scientific, Marlborough, MA), but the Exacto Cold Snare (Steris, Mentor, OH) is good, too. I work to ensure no mucosal islands and a wide resection margin of at least 3mm along the periphery of the lesion. I do not routinely use epinephrine in my injection solution because I have not found the mild oozing at the resection base to interfere with visualization nor cause sustained bleeding requiring intervention.
For future research: More data is needed to determine if an injection solution is required and whether piecemeal cold snare polypectomy is a suitable for SSLs with features of dysplasia, which could be particularly important for serrated polyposis syndrome patients with numerous lesions.
References
- Klein A, Bourke MJ. How to Perform High-Quality Endoscopic Mucosal Resection During Colonoscopy. Gastroenterology 2017;152:466-471.
- Crockett SD, Nagtegaal ID. Terminology, Molecular Features, Epidemiology, and Management of Serrated Colorectal Neoplasia. Gastroenterology 2019;157:949-966 e4.
- Kahi CJ, Hewett DG, Norton DL, et al. Prevalence and variable detection of proximal colon serrated polyps during screening colonoscopy. Clin Gastroenterol Hepatol 2011;9:42-6.
- Pohl H, Srivastava A, Bensen SP, et al. Incomplete Polyp Resection During Colonoscopy-Results of the Complete Adenoma Resection (CARE) Study. Gastroenterology 2012.
- Arain MA, Sawhney M, Sheikh S, et al. CIMP status of interval colon cancers: another piece to the puzzle. Am J Gastroenterol 2010;105:1189-95.
- Pellise M, Burgess NG, Tutticci N, et al. Endoscopic mucosal resection for large serrated lesions in comparison with adenomas: a prospective multicentre study of 2000 lesions. Gut 2017;66:644-653.
- Kemper G, Turan AS, Schoon EJ, et al. Endoscopic techniques to reduce recurrence rates after colorectal EMR: systematic review and meta-analysis. Surg Endosc 2021.
- Burgess NG, Bassan MS, McLeod D, et al. Deep mural injury and perforation after colonic endoscopic mucosal resection: a new classification and analysis of risk factors. Gut 2017;66:1779-1789.
- JE IJ, Bastiaansen BA, van Leerdam ME, et al. Development and validation of the WASP classification system for optical diagnosis of adenomas, hyperplastic polyps and sessile serrated adenomas/polyps. Gut 2016;65:963-70.

