ACG Comments: Protect Access to Care, Sanctity of Patient-Provider Relationship
Last week, ACG formally replied to the Senate Finance Committee’s report on Medicare Part B reforms, advancing our perspective on the dire financial and administrative challenges facing clinical gastroenterologists.
Our response highlighted ACG’s principles of Medicare reimbursement reform that we discussed with legislators during April’s Advocacy Day:
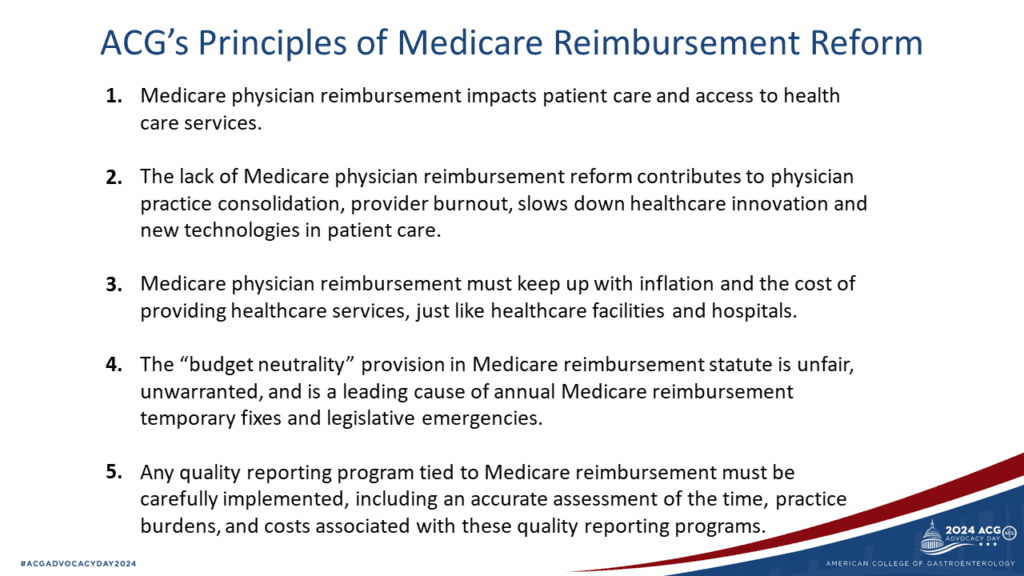
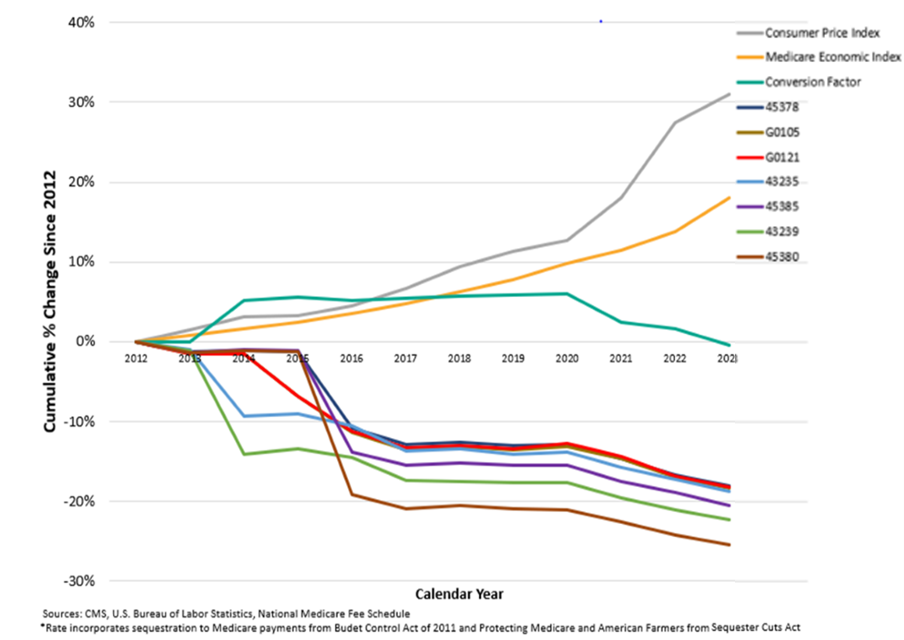
Next, we summarized the root causes of the current situation: Physicians, unlike hospitals and outpatient facilities, do not receive an annual inflationary adjustment to Medicare pay. This is only compounded by the budget neutrality requirement that requires any pay increase to one specialty’s service to come out of the pocket of another.
What does this look like for gastroenterology? This chart shows trends over the last decade of the consumer price index (a measure of inflation), the conversion factor, the Medicare Economic Index, and various GI codes for colonoscopy and endoscopy.
Finally, we reiterated to the committee that inaction on Medicare physician reimbursement and administrative burden reform are leading contributors to both practice consolidation and physician burnout.
According to a recent Medscape report, gastroenterology has among the highest burnout rates (50%). The top factors contributing to burnout remain bureaucratic tasks, hours spent at work, and government regulations. And that’s why our letter concluded with a plea to address MIPS reporting burdens, where CMS vastly underestimates the real costs of compliance – both time and financial.
Under the leadership of Louis Wilson, MD, FACG, the Legislative & Public Policy Council Chair, ACG continues to ring the alarm bells about the broken Medicare physician reimbursement system, urging a move from lip service to real action.
We invite you to review ACG’s full response to the Senate Finance Committee.
MedPAC’s June 2024 Report: MEI Adjustments, Site-Neutral Payments, and Prior Authorization in Medicare Advantage
Also last week, the Medicare Payment Advisory Commission (MedPAC) released its latest report to Congress. Without improvements to provider reimbursement, MedPAC cautioned, the future of physician participation in Medicare is at risk – which would significantly threaten patient access to care.
MedPAC officially came out in favor of an annual adjustment to the physician fee schedule that would be equal to the MEI, minus one percentage point.
While ACG was encouraged to see MedPAC recognize the need to increase physician pay by some inflationary measure, it was still insufficient. MedPAC again ignored the budget neutrality requirement and Congressionally-mandated spending cuts (e.g., sequestration, PAYGO) that would more than offset any positive MEI-based adjustment.
In addition, MedPAC restated its long-standing concern about the higher pay for services rendered in hospital outpatient departments compared to freestanding clinician offices. These so-called ‘site-neutral’ payment reforms could help stem the tide of vertical consolidation, the commission stated.
Finally, in a separate chapter, the commission dove into prior authorization in Medicare Advantage (MA). MedPAC found that 95% of the 37.5 million prior authorization requests made by providers in 2021 were approved, with 80% of appeals resulting in a favorable outcome (these rates are comparable to an HHS audit from 2019 data). Most importantly, we were pleased to see MedPAC is planning future research on the impact of these prior authorization requirements on care access, quality, and cost for MA beneficiaries.
For more details, please read MedPAC’s full June 2024 report, which includes a useful executive summary.

