Innovation and Technology in Gastroenterology and Hepatology
Highlights from the 2022 American College of Gastroenterology Annual Scientific Meeting Curated by the ACG Innovation & Technology Committee
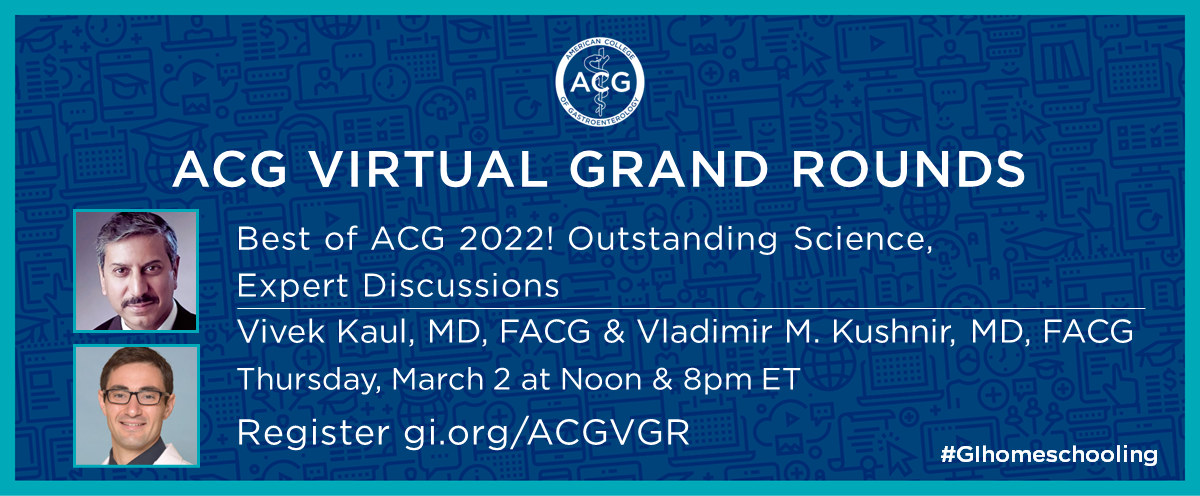
A recording of an ACG Virtual Grand Rounds on this topic is available:
Best of ACG 2022! Outstanding Science, Expert Discussions
March 2, 2023
Moderators: Vivek Kaul, MD, FACG and Vladimir M. Kushnir, MD
Presenters: Amer AlSamman, MD; Adam Buckholz, MD, MS; Daniel Castaneda, MD; Sarah M. Enslin, PA-C; Daniela Guerrero Vinsard, MD
Panelists: Prabhleen Chahal, MD, FACG; Jean Chalhoub, MD; Ryan B. Perumpail, MD; Aparna Repaka, MD
The ACG Innovation and Technology Committee is tasked with fostering creativity and innovation in our specialty and working with ACG members and industry in the development of meaningful technology, new techniques and promoting novel research with the ultimate goal of improved patient care.
The ACG Annual Scientific Meeting is a unique, internationally recognized platform to showcase these efforts. At the ACG Annual Scientific Meeting & Postgraduate Course for 2022 held in Charlotte, NC, colleagues were able to congregate and attend safely in person once again and present their latest research and science as well as attend several high-quality educational sessions. Several members of the ACG Innovation & Technology committee have helped collate a brief summary of selected scientific papers, highlighting the latest innovation and technology presented at ACG 2022.
We hope you find this condensed review helpful!
Innovations in Pharmacotherapeutics
Inflammatory Bowel Disease
Brian G. Feagan, MD; Gareth Parkes, DO; Pascal Juillerat, MD; Krisztina Gecse, MD; Xuan Yao, PhD; Wen Zhou, MD, PhD; Huiwen Deng, PharmD; Dapo Ilo, MBBS, MRCS, MSc; Yuri Sanchez-Gonzalez, PhD; Peter D. Higgins, MD, PhD, MSc
Feagan, et al. presented post-hoc results of the phase 3 upadacitinib (UPA) U-ACHIEVE study for ulcerative colitis. Patients responding to 45 mg induction for 8 weeks with UPA (n=451) were randomized to 30 mg, 15 mg and placebo and were followed for 52 weeks. Higher clinical remission was seen in patients on either 30 or 15 mg UPA compared to placebo (34.4 and 30.5% versus 15.8%), determined by the Adapted Mayo score. Patients on 30 mg dosing showed milder disease at the end of the 52 weeks compared to patients on 15 mg dosing, as well as higher remission rates.
The American Journal of Gastroenterology 117(10S):p e496, October 2022. | DOI: 10.14309/01.ajg.0000859488.03460.db
Edouard Louis, MD; Joana Torres, MD, PhD; James Lindsay, DO; Stefan Schreiber, MD; Ryan Ungaro, MD, MS; Laimas Jonaitis, MD, PhD; Kristina Kligys, PhD; Stijn Van Haaren, MsC; Ezequiel Neimark, MD; Javier Zambrano, MD; Yafei Zhang, PhD; Geert D’Haens, MD
Louis, et al. presented a post hoc analysis of the efficacy and safety of Risankizumab, an anti-IL23 monoclonal antibody, for moderate to severe Crohn’s disease in patients who have failed or were in tolerant to prior biologic therapy. Data was obtained from the ADVANCE, MOTIVATE and FORTIFY studies. 450 patients were randomized 1:1:1 to receive RZB 360mg vs RZB 180mg vs placebo. 48% of patients previously failed 1 biologic, 25% failed 2, and 27% of patients failed >3 prior biologics. Induction and maintenance treatment were well-tolerated consistent with prior reports. RZB was effective in all patients regardless of the number of prior biologics failed although highest success was seen in patients who failed <2 biologics. Of note, patients who failed >2 biologic agents had higher chance of achieving endoscopic endpoints with the higher dose of RZB (360mg) vs 180mg RZB and placebo.
The American Journal of Gastroenterology 117(10S):p e496-e497, October 2022. | DOI: 10.14309/01.ajg.0000859492.75431.51
Esophagus
Ronnie Fass, MD; Michael F. Vaezi, MD; Prateek Sharma, MD; Rena Yadlapati, MD, MS; Barbara Hunt, MSc; Tom Harris, BSc; Neila Smith, MD; Eckhard Leifke, MD; David Armstrong, MA, MBBCh, FACG
Fass, et al. presented a phase 2 study evaluating the efficacy and safety of vonoprazan for on-demand management of non-erosive reflux disease. All patients (n=207) were initially given vonoprazan 20 mg daily for a week and were subsequently randomized to vonoprazan 10 mg, 20 mg, 40 mg or placebo as needed for 6 weeks. Vonoprazan was superior to placebo in achieving symptom relief at all three doses. Higher rates of symptom relief were achieved with 40 mg compared to 10 and 20 mg dosing (70% versus 60.6% and 56%, respectively).
The American Journal of Gastroenterology 117(10S):p e272-e273, October 2022. | DOI: 10.14309/01.ajg.0000858200.17525.4a
Evan Dellon, MD, MPH; Marc Rothenberg, MD, PhD; Albert Bredenoord, MD, PhD; Alfredo Lucendo, MD; Ikuo Hirano, MD, PhD; Xian Sun, PhD; Kiran Patel, PhD; Bethany Beazley, PhD
Dellon, et al. presented the phase 3 randomized controlled trial results of dupilumab for the management of eosinophilic esophagitis. Dupilumab, an IL-4 and IL-13 monoclonal antibody antagonist, was compared to placebo in a cohort of 240 patients, which were randomized in a 1:1 fashion and followed for 24 weeks. Patients on dupilumab achieved in higher proportion an eosinophil count ≤6/hpf at follow up (59% vs 5.9%, p <0.001) and change in the absolute and percentage Dysphagia Symptom Questionnaire scores. There was also statistical difference between both groups in the improvement of endoscopic reference score and histologic scoring system, favoring dupilumab over placebo. Dupilumab was safe, with the most common adverse effect being injection-site reaction (33.3%).
The American Journal of Gastroenterology 117(10S):p e269-e270, October 2022. | DOI: 10.14309/01.ajg.0000858188.99771.64
Liver
Mirna Kaafarani, BS; Omar Shamaa, MD; Syed-Mohammed Jafri, MD
Kaafarani, et al. presented a case series of patients with severe aortic stenosis, often an immovable barrier to transplant. In their cohort, correcting the aortic stenosis with minimally invasive TAVR allowed two patients to be successfully transplanted with good graft function at a median of 27 months follow up. There is a paucity of data on this topic. This case series suggests that addressing underlying significant valvular heart disease may lead to sufficient cardiovascular recovery to permit liver transplant.
The American Journal of Gastroenterology 117(10S):p e1894, October 2022. | DOI: 10.14309/01.ajg.0000868280.55869.50
Khurram Jamil, MD; Ethan Weinberg, MD; Rajender Reddy, MD, FACG
Jamil, et al. presented a subgroup analysis from the CONFIRM randomized, placebo-controlled study, evaluating whether terlipressin (TERLI) therapy reduced the need for renal replacement therapy (RRT) and improved overall survival through 12 months in liver transplant recipients. 75 patients who underwent liver transplantation were included in the study (46 patients received TERLI + albumin, 29 patients received albumin alone). HRS reversal was significantly higher in the TERLI group vs PBO (37% vs 14%, p=0.021). The need for RRT was significantly lower in the TERLI group vs placebo in both the pre-transplant and post-transplant phases (p=0.017 and p=0.009, respectively). Overall survival was similar (94% vs 93%, p=0.93).
The American Journal of Gastroenterology 117(10S):p e853, October2022. | DOI: 10.14309/01.ajg.0000861332.82608.85
Stomach
David Cangemi, MD; Marilia Montenegro, MD; Brennan Spiegel, MD; Brian E. Lacy, MD, PhD, FACG
Cangemi, et al. presented a randomized, controlled, double-blinded study of 37 patients with functional dyspepsia by Rome IV criteria randomized 2:1 to receive either an immersive audiovisual program with virtual reality (n=27) vs control with 2-D nature videos (n=10). Patients in each arm used the virtual reality (VR) headset at least once daily for 2 weeks (average 1.3 times/day, mean 23.2 minutes/day). Mean PAGI-SYM scores decreased and NDI QOL scores increased for all patients, with greater effect seen in the VR group. 17 patients reported non-serious AEs (headache, dizziness). 1 patient withdrew from the study due to migraine headaches. This study suggests VR may be an effective therapeutic treatment option in functional dyspepsia. Large validation studies are needed.
The American Journal of Gastroenterology 117(10S):p e365, October 2022. | DOI: 10.14309/01.ajg.0000858696.28989.d8
Irene Sarosiek, MD; Ryan Torelli; Mohammad Bashashati, MD; Jesus Diaz, MD; Oswaldo Padilla, MD; Bright Tamis, MD; Sherif E. Elhanafi, MD; Brian Davis, MD; Richard W. McCallum, MD
Sarosiek, et al. presented results from a randomized double blind placebo control trial evaluating surgical pyloroplasty (SP) and gastric electrical stimulation (GES) vs pyloroplasty (PP) alone for management of gastroparesis. 30 patients with drug-refractory gastroparesis underwent simultaneous surgical implantation of the GES system and PP. Patients were randomized to active GES stimulation vs no stimulation for 3 months. Both cohorts had improved gastroparesis cardinal symptom index (GCSI) scores compared to baseline at 3 months (p<0.01), however the GES-on group had significantly better mean improvement vs GES-off group. All patients had GES turned on from months 3-6 with significant improvement in the GCSI in the GES-off group. Hospitalizations due to vomiting were significantly reduced in the GES-ON group vs GES-OFF group (p=0.02). Interestingly there were no technical dysfunctions or post-surgical complications reported.
The American Journal of Gastroenterology 117(10S):p e1131, October 2022. | DOI: 10.14309/01.ajg.0000862980.76605.08
Colon
Sahil Khanna, MBBS, MS, FACG; Paul Feuerstadt, MD, FACG; Edward Huang, MD, MPH; Caterina Oneto, MD; Darrell S. Pardi, MD, MS, FACG; Elaine E. Wang, MD; Ananya De, PhD; Kelly Brady, MD; Asli Memisoglu, PhD; David Lombardi, PhD; Brooke Hasson, PhD; Barbara McGovern, MD; Lisa Von Moltke, MD
Khanna, et al. presented a phase 3, open label, single-arm study evaluating the use of SER-109, an investigational microbiome of purified Firmicutes spores, in adults with recurrent Clostridioides difficile infection (rCDI). 263 patients were enrolled into 2 cohorts: 29 patients from ECOSPOR III study with rCDI (cohort 1) and 234 patients with >1 CDI recurrence. Patients received standard of care antibiotic therapy followed by SER-109 4 capsules once daily x 3 days. Safety and efficacy were assessed through 8 weeks and durability of response was assessed through 24 weeks. SER-109 was well-tolerated. Rates of rCDI after SER-109 were low regardless of number of prior CDI episodes (8.7% at week 8, 13.7% at week 24).
The American Journal of Gastroenterology 117(10S):p e96-e97, October 2022. | DOI: 10.14309/01.ajg.0000857172.24140.48
Darren M. Brenner, MD, FACG; Carol Rockett, PharmD; Mansi Jamindar, PharmD; Enoch Bortey; June Almenoff, MD, PhD; Brooks D. Cash, MD, FACG
Brenner, et al. presented results from a pooled analysis of 2 global phase 2 studies of naloxegol for treatment of opioid-induced constipation (OIC). 1337 patients received either naloxegol 25mg, naloxegol 12.5mg or placebo. Naloxegol was superior to placebo at achieving clinically meaningful symptom improvement at both thresholds (minimal clinically important difference thresholds of 0.5 and 0.8). Improvement was dose dependent, with highest improvement seen in the naloxegol 25mg cohort.
The American Journal of Gastroenterology 117(10S):p e117-e118, October 2022. | DOI: 10.14309/01.ajg.0000857296.33937.6e
Innovations in Endoscopy
General Endoscopy
Cátia Arieira, MD; José Cotter, MD; Ricardo Gorjão, MD; Vicente Lorenzo-Zúñiga, MD; Miguel A. Pantaleón Sánchez, MD; David Carral Martínez, MD; Fernándo Sábado, MD; Elena Pérez Arellano, MD; Blas J. Gómez Rodríguez, MD; Antonio López Cano, MD; Salvador Machlab, MD; Jose M. Esteban López-Jamar, MD; Elena Velasco, MD; Sarbelio Rodriguez, MD; Juha Halonen, PhD; Fatma Akriche, MD; Carmen Turbí Disla, MD
Arieira, et al. presented a multicenter, observational study of > 13,000 patients evaluating the use of 1L polyethylene glycol + ascorbic acid (1L PEG + ASC) for colonoscopy bowel preparation. Patients completed bowel preparation with 1L PEG + ASC as either split dose or same-day regimen. Adequate bowel prep, defined as total Boston Bowel Preparation Scale (BBPS) > 6 with all segmental scores > 2, was achieved in 89.3% of patients. High-quality cleansing, defined as segmental BBPS scores of 3, was achieved in 49.3% of patients. Split dose regimen was superior to same-day for adequate prep (94.7% vs 86.7%, p<0.0001) and for high-quality right colon prep (65.4% vs 41.4%, p < 0.0001). Incomplete colonoscopy due to poor bowel prep occurred in only 0.8% of patients. Adverse events occurred in 2.3% (nausea 1.2%, vomiting 0.8% and abdominal pain 0.2%).
The American Journal of Gastroenterology 117(10S):p e415-e416, October 2022. | DOI: 10.14309/01.ajg.0000858996.89487.6e
Therapeutic Endoscopy
Abhishek Agnihotri, MD; Divya Chalikonda, MD; Daniel Scanlon, BA; Anand Kumar, MD, MPH; Alexander Schlachterman, MD
Agnihotri, et al. compared the use of a new through the scope steerable grasper (SGA) to the traditional clip and line technique (C&L) during ESD performed by novice endoscopists. The authors performed a prospective, single center randomized trial that recruited 10 novice endoscopists with 1-3 years of experience but no prior ESD experience. Each subject performed two ESD procedures, each on a 25 mm circular lesion in an ex-vivo porcine stomach model. Endoscopists were randomized to either perform ESD with SGA first, followed by the C&L method, or vice versa. Mean dissection time was shorter when using SGA compared to the C&L technique, irrespective of the order of randomization (5.07 + 2.19 mins vs 20.07 + 8.45 mins, P< 0.001). The rate of muscle injury and perforation was also lower in the SGA group (1 vs. 4 with the C&L technique). Interestingly, the use of SGA was associated with significantly lower NASA task load index scores across the domains of mental, physical, and temporal demands, performance, effort, and frustration. All participants preferred SGA over C&L methods. The study suggests that for novice endoscopists performing ESD with access to a double-channel therapeutic endoscope, the SGA could be a valuable tool to improve their learning curve and efficiency with this delicate and challenging procedure.
The American Journal of Gastroenterology 117(10S):p e781, October 2022. | DOI: 10.14309/01.ajg.0000860948.90894.50
Scott R. Douglas, MD; Douglas K. Rex, MD, MACG; Alessandro Repici, MD; Melissa Kelly, BSN, RN, CGRN; Wes Heinle, MPH; Matthew T. Moyer, MD, MS
Douglas, et al. performed a multicenter, international, retrospective study demonstrating the safety and efficacy of Distal Cap-Assisted Endoscopic Mucosal Resection (EMR-DC) for managing adherent and non-lifting colon polyps. 61 EMR-DC cases performed by three expert endoscopists for non-lifting colon polyps due to submucosal fibrosis from previous biopsy, tattoo, or attempted resection were included in the study. EMR-DC was preceded by attempted polypectomy or EMR in 88.5%, submucosal tattoo injection in 1.6%, prior biopsy in 4.9% and both biopsy and tattoo in 4.9% of cases. Complete macroscopic resection was achieved in 100% of EMR-DC. Lesion size ranged from 15mm to 95mm (average: 49mm). Procedure time averaged 49.5 minutes. The adenoma recurrence rate for these complex and adherent lesions at six-month surveillance was only 9.8%. Two serious post-procedural adverse events occurred (3.3%): one post-procedural bleeding requiring repeat colonoscopy and one episode of post-polypectomy syndrome requiring hospitalization. This large, multicenter series demonstrates EMR-DC to be a safe and efficacious approach to a difficult and common clinical problem – adherent and non-lifting polyps.
The American Journal of Gastroenterology 117(10S):p e94-e96, October 2022. | DOI: 10.14309/01.ajg.0000857160.20906.1f
Biliary/Pancreas
Jad AbiMansour, MD; Rabih Ghazi, MD; Andrew C. Storm, MD; Michael J. Levy, MD; John A. Martin, MD; Ryan Law, DO; Eric J. Vargas, MD, MS; Barham Abu Dayyeh, MD, MPH; Bret T. Petersen, MD; Vinay Chandrasekhara, MD
AbiMansour, et al. performed a retrospective study comparing fully covered (FC-SEMS) and uncovered (UC-SEMS) self-expandable metal stents [WallFlex (Boston Scientific, Boston, MA) and Flexxus (ConMed, Utica, NY)] in the management of malignant biliary obstruction due to locally advanced pancreatic cancer. The majority of the cohort had an UC-SEMS placed [152 (81.3%)] and were followed for a mean of 15.6 months (Range: 8.8 – 24.6). FC-SEMS was deployed in 35 patients (18.7%) who were followed for a mean of 22.4 months (Range: 8.3 – 27.9). The primary outcomes were (1) clinical success defined as a reduction in bilirubin by 33% in 1 week, 50% within 2 weeks, or resolution of obstruction, (2) adverse events (AEs), and (3) need for unplanned re-intervention to manage stent-related AEs. Both stents achieved significantly high clinical success (92.1% UCSEMS vs. 97.1% FCSEMS, p = 0.29). Regarding AEs, there were higher stent occlusion rates due to tumor ingrowth with UC-SEMS [(44 (28.9%) vs. 1 (2.9%), p = 0.001)] justifying longer patency times with FC-SEMS. There was no difference in the rates of other AEs: post-ERCP pancreatitis, stent migration, and cholecystitis. The use of FC-SEMS was associated with a significantly lower rate of unplanned interventions as compared to the use of UC-SEMS [2 (6%) vs. 44 (29%), p < 0.05]. No difference in surgical resection rates, time to stent occlusion, time to unplanned reintervention, duration of survival, and mortality rates between the two groups. Despite the retrospective design and the small number of patients in the FC-SEMS group, the study suggests that FC-SEMS use leads to fewer reinterventions and potentially lower costs, as well as improved palliation in patients with distal biliary obstruction secondary to pancreatic cancer.
The American Journal of Gastroenterology 117(10S):p e61-e62, October 2022. | DOI: 10.14309/01.ajg.0000856972.84000.5a
Muhammad Salman Faisal, MD1, Mauricio Columbus-Morales, MD1, Omar Shamaa, MD2, Cyrus Piraka, MD1, Andrew Watson, MD1, Robert Pompa, MD1, Duyen Dang, MD1, Tobias Zuchelli, MD1, Sumit Singla, MD2
Faisal, et al. performed a retrospective study to evaluate the safety of cholangioscopy in patients with PSC. 89 patients were included, 28 underwent ERCP with cholangioscopy, 61 underwent ERCP only. There were no demographic differences between the two groups, including the number of patients with cirrhosis and cholangiocarcinoma. Similarly, the two groups were comparable in terms of their ERCP findings, interventions, and complications. Interestingly, the rate of infection or cholangitis was higher in patients undergoing ERCP alone [7 (11.5%)] compared to the ERCP and cholangioscopy group [1 (5%)] but that did not achieve a statistical significance (p = 0.67). As expected, median total procedure time was higher in the ERCP and cholangioscopy group (90 vs. 70 mins with ERCP alone); that did not reach statistical significance likely due to the small sample size. Cholangioscopy use did not affect the median fluoroscopy time (10.4 vs 11.5 mins with ERCP alone, p = 0.59). This study suggests that ERCP with cholangioscopy is safe in patients with PSC but larger prospective studies are needed.
The American Journal of Gastroenterology 117(10S):p e59-e60, October 2022. | DOI: 10.14309/01.ajg.0000856960.18186.42
Wasef Sayeh, MD; Azizullah A. Beran, MD; Sami Ghazaleh, MD; Mohammad Safi, MD; David Farrow, MD; Sudheer Dhoop, MD; Rami Musallam, MD; Justin Chuang, MD; Saif-Eddin Malhas, MD; Waleed Khokher, MD; Omar Sajdeya, MD; Anas Renno, MD; Muhammad Aziz, MD; Yaseen Alastal, MD, MPH
Sayeh, et al. performed a systematic review and meta-analysis on studies comparing endoscopic ultrasound (EUS)-guided fine needle aspiration (FNA) and EUS through the needle biopsy (TTNB) for adequate sampling and diagnostic accuracy in patients with pancreatic cystic lesions (PCLs). Nine observational studies involving 520 patients were included. The rate of sample adequacy was significantly higher in the EUS-TTNB group compared to the EUS-FNA group (RR 1.64, 95% CI 1.19-2.26, p =0.003, I2 = 95%). Only four studies compared the accuracy rate between the EUS-TTNB method and the EUS-FNA group. Diagnostic accuracy was significantly higher in the EUS-TTNB group compared to the EUS-FNA group (RR 2.03, 95% CI 1.13-3.65, p = 0.02, I2 = 87%). The authors concluded that EUS-TTNB should be considered where applicable clinically for improving the diagnostic yield in patients undergoing evaluation of PCLs.
The American Journal of Gastroenterology 117(10S):p e34-e35, October 2022. | DOI: 10.14309/01.ajg.0000856824.07133.76
Ishani Shah, MD; Andy Silva-Santisteban, MD; Katharine A. Germansky, MD; Rishi Pawa, MBBS; Vladimir Kushnir, MD; Arvind Trindade, MD; Jiannis Anastasiou, MD; Kara L. Raphael, MD; Girish Mishra, MD; Sumant Inamdar, MD; Benjamin Tharian, MD; Mandeep S. Sawhney, MD
Shah, et al. presented results from a prospective, multicenter study (Pancreas Scan study) of 252 high-risk patients undergoing pancreas cancer screening. Patients underwent either EUS (n=208) or MRI (n=44). High risk pathology was found in 0.8%, intermediate risk in 31.7% and low risk in 23.4% of patients. Two patients were diagnosed with pancreatic cancer (T2N1M0, treated with neoadjuvant chemotherapy and pancreatic resection; T2N1M1 treated with palliative chemotherapy). There were no adverse events. Further long-term data is needed to evaluate the yield and outcomes of pancreas cancer screening.
The American Journal of Gastroenterology 117(10S):p e1, October 2022. | DOI: 10.14309/01.ajg.0000856644.27737.00
Umar Hayat, MBBS; Cyrus Munguti, MD; Muhammad Kamal, MD; Muhammad Haseeb, MD, MSc
Hayat, et al. presented a systematic review and meta-analysis of 13 studies (1339 patients) who underwent treatment of malignant biliary strictures with radiofrequency ablation (RFA) + stenting vs stenting alone. Stent patency was preserved longer in the RFA + stent group with pooled weighted mean difference in stent patency of 43.5 days. Overall survival also favored the RFA + stent group with pooled weighted mean difference of 90.53 days. No significant difference was seen in rate of adverse events between the 2 groups.
The American Journal of Gastroenterology 117(10S):p e14-e15, October 2022. | DOI: 10.14309/01.ajg.0000856708.31470.07
New Techniques and Care Pathways
Clinical Applications of Artificial Intelligence
Tiago Ribeiro, MD; Miguel Mascarenhas, MD; Joao Afonso, MD; Filipe Vilas-Boas; João Ferreira, PhD; Pedro Pereira; Guilherme Macedo, MD, PhD
Ribeiro, et al. explored the use of artificial intelligence (AI) for the evaluation of neoplastic biliary nodules in patients with indeterminate biliary strictures. The authors designed a convolutional neural network for automatic identification of biliary nodules based on data from 16,150 frames taken from a pool of 85 patients undergoing cholangioscopy. The frames were classified by two experienced endoscopists, two datasets were built for training and validation, and the architecture of the network was optimized for the detection of malignant biliary nodules.The software achieved promising results with a sensitivity of 94%, specificity of 99.9%, PPV of 98.8%, and NPV of 99.7%, and overall accuracy of 99.6%. The study suggests that in patients with indeterminate biliary strictures, AI-assisted cholangioscopy could help improve the yield of intraductal biopsies, potentially expediting the diagnosis and management of concerning biliary strictures. Further studies integrating cholangioscopic and histologic findings are needed to validate this model.
The American Journal of Gastroenterology 117(10S):p e20, October 2022. | DOI: 10.14309/01.ajg.0000856740.48694.91
Jose D. Debes, MD, PhD; David Jonason, MD; Tiancong Cheng, BS; Ju Sun, PhD
Debes, et al. presented a retrospective evaluation of 142 abdominal ultrasound examinations, evaluating whether portal vein with sound wave assessment can aid in HCC detection. AI was used to identify doppler signatures consistent with HCC. The AI was trained with 80% of samples and tested on 20%. The test sample found that those doppler signatures predicted tumor presence. The average size tumor was relatively small (2.8 cm), with an AUROC of 0.85 at 20 ng/mL. When combined with AFP, the AUROC improved to 0.96. While further validation is needed, this data suggests AI for sound analysis may help improve the detection of cancer.
The American Journal of Gastroenterology 117(10S):p e859, October 2022. | DOI: 10.14309/01.ajg.0000861360.44966.6d
Weiquan James Li, MBBS, MMed; Clement Wu, MBBS, MRCP; Christopher Jen Lock. Khor, MBBS; Raymond FH. Liang, MBBS, MRCP; Jonathan Wei Jie Lee, MBBS, MRCP; Jimmy So, MBChB, FRCSEd, FRCSG, FAMS, MPH; Weida Chew, MBBS, MRCP
Li, et al. presented interim analysis of a prospective multicenter study evaluating the use of AI in characterization of colon polyp histology. 625 polyps were detected in 257 patients (303 hyperplastic, 322 neoplastic). The CADx (Fujifilm Corp, Tokyo) achieved sensitivity for diagnosis of hyperplastic polyps of 84.2% vs 77.6% for CADx and endoscopist. Similar performance was seen in the evaluation of diminutive polyps (81.7% vs 76.3%). This study suggests CADx may have superior performance to endoscopists in the prediction of hyperplastic polyp histology during endoscopy. Large prospective studies are needed to evaluate further.
The American Journal of Gastroenterology 117(10S):p e99, October 2022. | DOI: 10.14309/01.ajg.0000857184.76822.9c
Miguel Mascarenhas, MD; Lucas Spindler, MD; Nadia Fathallah, MD; Tiago Ribeiro, MD; Joao Afonso, MD; João Ferreira, PhD; Guilherme Macedo, MD, PhD; Vincent De Parades, MD, PhD
Mascarenhas, et al. developed an AI system for automatic detection and differentiation of high grade versus low grade squamous intraepithelial anal lesions in high resolution anoscopy (HRA) images. The system was developed using 5026 images (1517 images containing HSIL and 3509 LSIL) from 78 HRA exams done between January 2021 and January 2022. The test set comprised 10% of the images. The system had an overall accuracy of 92.3%. The CNN had sensitivity, specificity, positive and negative predictive values of 91.4%, 92.7%, 86.9%, and 95.9%, respectively. The area under the curve was 0.97. This study demonstrates the successful development of an algorithm for automated classification and detection of anal squamous cell carcinoma precursors with a great performance and almost perfect AUC. This tool, if externally validated, has a potential to facilitate prompt diagnosis and treatment, potentially bypassing histopathological diagnosis.
The American Journal of Gastroenterology 117(10S):p e97-e98, October 2022. | DOI: 10.14309/01.ajg.0000857176.10120.1e
Artificial Intelligence in Healthcare Operations/Practice Management:
Joseph D. Feuerstein, MD; Samuel Miller, MD; Michelle Ladonne, MHA, CMPE; Arvind Ravi, MD, PhD
Feuerstein, et al. describe the use of an artificial intelligence system to identify high risk patients potentially overdue for repeat colonoscopy during the COVID-19 pandemic and to investigate the reasons for missed surveillance within 2 years. A natural language tool (NLP) was developed to convert procedure reports to text files and these reports were evaluated alongside electronic healthcare records (EHR) by the investigators to determine the timing and indication of the surveillance procedure. 677 cases had a recommendation for surveillance within 2 years, 24% (n=162) were flagged as potentially overdue. Of the 162 cases, 48 had missing colonoscopy orders, 31 were not contacted by scheduling, and 32 were lost to follow up despite at least 1 attempted outreach. The remaining 51 were also lost to follow up but not deemed overdue (had colonoscopy elsewhere, passed away, etc). This study highlights the use of NLP for automated identification of patients overdue for colonoscopy for various reasons. Such system has the potential of flagging these cases with an opportunity for intervention and optimization of surveillance compliance in patients at risk for colorectal cancer.
The American Journal of Gastroenterology 117(10S):p e221, October 2022. | DOI: 10.14309/01.ajg.0000857868.62929.a2
Artin Galoosian, MD, MA; Jamie O. Yang, MD; Emma Peterson, MS; Cleo K. Maehara, MD, MMSC; Jayraan Badiee, MPH; Camille Soroudi, MD; Anthony Myint, MD; Yuna Kang, MD; Bita V. Naini, MD; Sadie De Silva, MD; V. Raman Muthusamy, MD, MAS, FACG; Eric Esrailian, MD, MPH; William Hsu, PhD; Folasade P. May, MD, PhD, MPhil
Galoosian, et al. developed and validated a natural language processing (NLP) tool to automatically measure 4 intraprocedural colonoscopy quality improvement (QI) metrics: colonoscopy indication (IND), bowel preparation (BP), cecal intubation (CI), and successful cecal intubation (SCI). They compared the performance of NLP to automatically classify these variables versus the gold standard chart review by humans. For all metrics, sensitivity of the NLP system ranged from 99.3 to 100.0% and specificity ranged from 94.3 to 100.0%. Compared to humans, NLP misclassified 15 cases (2 IND, 1 BP and 12 SCI). These were mostly due to conflicting documentation by the endoscopist in the endoscopy report. This study explores the use of NLP for automated collection of colonoscopy quality metrics. An automated NLP system would have the advantage of collecting a large amount of quality data in a short time span, saving hours of work by humans. However, further improvements in the pipeline, including a more accurate documentation by endoscopists along with further refinement of the NLP tool, need to be achieved before this tool can be implemented.
The American Journal of Gastroenterology 117(10S):p e204-e205, October 2022. | DOI: 10.14309/01.ajg.0000857780.82735.33

