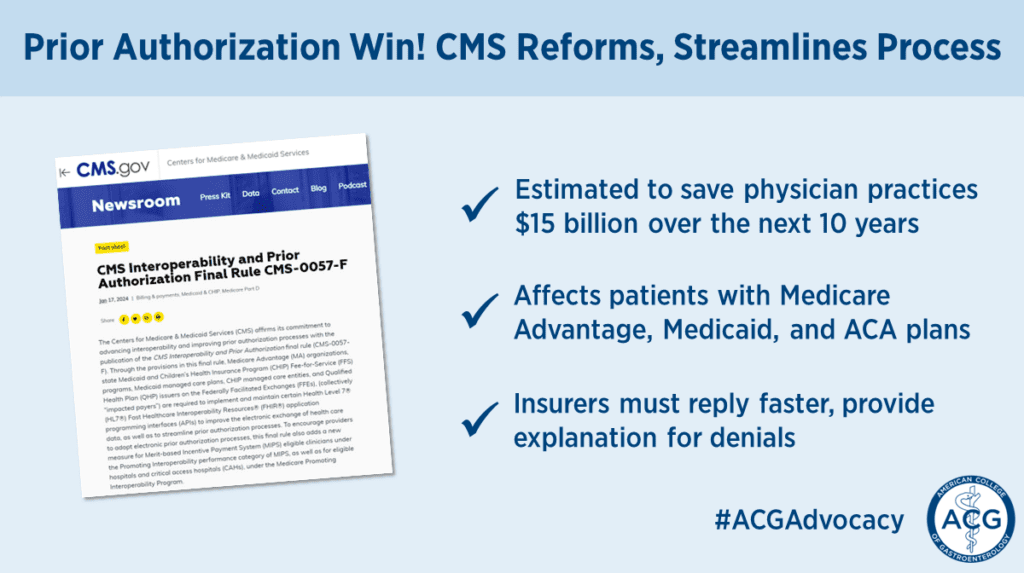
In a significant win for ACG members and healthcare providers, the Centers for Medicare & Medicaid Services (CMS) finalized a rule that reforms the prior authorization process for services, while easing physician reporting burdens.
The Advancing Interoperability and Improving Prior Authorization Processes (e-PA) rule (CMS-0057-F) applies to Medicare Advantage organizations, state Medicaid and CHIP programs, and commercial insurers regulated by the Affordable Care Act (ACA) marketplaces.
CMS estimates that the new suite of reforms will save physician practices $15 billion over the next 10 years. ACG is grateful for our membership’s successful advocacy in speaking from experience and educating policymakers on the administrative burdens of prior authorization on gastroenterologists – not to mention the adverse impact on patient care.
We are also pleased to see the rule is consistent with the provisions and objectives of the Improving Seniors’ Timely Access to Care Act, which provides an expedited prior authorization review and additional guardrails for the Medicare Advantage program. In recent years, ACG leaders have advocated for this legislation during our annual advocacy day in Congress.
Here’s what you need to know about the new regulation:
1. Services, not drugs
The rule applies to durable medical equipment and medical procedures and services, but not to drugs. ACG recognizes that this is a critical gap in this policy change and continues to advocate for broader reforms for drugs and biologics.
While our advocacy in this area is ongoing, ACG also offers membership tools to help your patients access care and reduce the burdens of prior authorization for your practices. Members should take advantage of our prior authorization letter generator tool – create custom letters tailored to your patient’s needs now!
2. Improved response times, explanations
CMS is requiring impacted payers (excluding ACA regulated plans) to send prior authorization decisions within 72 hours for expedited (i.e., urgent) requests and 7 calendar days for standard (i.e., non-urgent) requests.
Payers must also provide a specific reason for denied prior authorization decisions, regardless of the method used to send the prior authorization request. These requirements begin in January 2026.
3. Electronic streamlining
The rule also requires payers to implement a Health Level 7 (HL7®) Fast Healthcare Interoperability Resources (FHIR®) Prior Authorization application programming interface (API), which can be used to facilitate a more efficient process between providers and payers. Medicare Fee For Service has already implemented an API for prior authorization.
The API must contain its list of covered items and services, documentation requirements for approval, and information on the decision. The Provider API will allow providers to retrieve patient claims, encounter, clinical, and prior authorization data.
Payers will be required to expand patient access to the API, as well as implement a payer-to payer API. These requirements begin in January 2027.
4. Required prior authorization metric reporting
Payers are required to publicly report certain prior authorization metrics annually by posting them on their website, with the initial set of metrics be reported by March 31, 2026.
5. New MIPS measure
CMS is adding a new measure, titled “Electronic Prior Authorization,” to the MIPS Promoting Interoperability performance category. MIPS eligible clinicians will report the Electronic Prior Authorization measure beginning with the Calendar Year (CY) 2027 performance period/CY 2029 MIPS payment year.
ACG continues to view prior authorization as practicing medicine without a medical license.
More comprehensive prior authorization reforms remain a key public policy priority for ACG, but we are encouraged that the administration listened to providers in issuing the new regulation.
But for now, thank you again to the many ACG members who helped us generate momentum on this issue!

