Hepatic Decompensation Rate Is 0.05 per 100 person-years in NAFLD with Stage F0-F2 Fibrosis, but Rises to 1 per 100 person-years with Stage F3
 Philip Schoenfeld, MD, MSED, MSc (Epi)1 and Sonali Paul, MD, MS2
Philip Schoenfeld, MD, MSED, MSc (Epi)1 and Sonali Paul, MD, MS2
1Chief (Emeritus)-Gastroenterology Section, John D. Dingell VA Medical Center, Detroit, Michigan
2Assistant Professor of Medicine, Center for Liver Disease, Division of Gastroenterology, Hepatology & Nutrition, University of Chicago School of Medicine, Chicago, Illinois
This article reviews Sanyal AJ, Van Natta ML, Clark J, et al. Prospective Study of Outcomes in Adults with Nonalcoholic Fatty Liver Disease. N Engl J Med 2021; 385: 1559-69. DOI: 10.1056/NEJMoa2029349. PMID: 34670043
Correspondence to Philip Schoenfeld, MD, MSED, MSc (Epi), Editor-in-Chief, Associate Editor. Email: EBGI@gi.org
portal fibrosis; F3-bridging fibrosis; F4-cirrhosis, and 30% had F3/F4 fibrosis score. Study patients had minimal or no alcohol consumption based on answers to the Alcohol Use Disorders Identification Test questionnaire. Patients received standard of care at their NASH Clinical Research Network center.
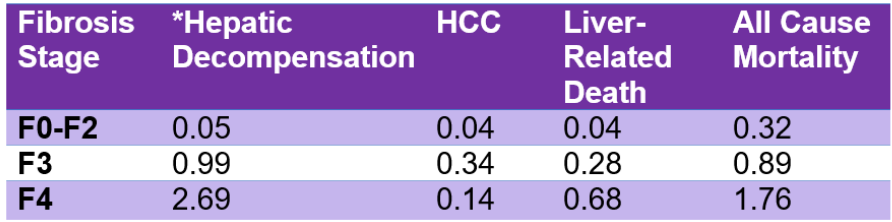
Table 1. Rates of hepatic and non-hepatic outcomes in NASH patients (per 100 person-years of follow-up) *Hepatic decompensation: clinically apparent ascites, overt encephalopathy, or variceal hemorrhag
_______________________________________________________________________
COMMENTARY
Why Is This Important?
NAFLD, which is a complex metabolic disorder closely linked to obesity and type 2 diabetes mellitus, is present in more than a quarter of the adult population.1 NASH, the progressive form of NAFLD, has surpassed hepatitis C as the primary cause of cirrhosis and is present in 5% of the US population.2 With the ongoing epidemic of obesity in the US, the prevalence of NASH will continue to grow. Management of patients with NAFLD includes education about the incidence of hepatic decompensation and HCC. Previously, these estimates came from retrospective analyses. Data from the NASH Clinical Research Network and this specific study are prospective, utilize liver histology to determine fibrosis score, and adhere to STROBE guidelines for optimal design and reporting about prospective cohort studies.3 Thus, this study provides precise data about prognosis and supplements the most recent guidelines about NAFLD management.4
Key Study Findings
In multivariate logistic regression models, new hepatic decompensation was the only factor associated with increased risk of all-cause mortality. Rates of hepatic decompensation are very small among patients with stage F0-F2 fibrosis (0.05 per 100 person-years), but increase significantly with stage F3 fibrosis (0.99 per 100 person-years, crude hazard ratio = 18.6; 95% CI: 5.4-62.6).
Caution
Study patients were primarily White and of European descent (85%), so it’s unclear if outcomes are different in African-Americans. Fibrosis stage was determined by liver biopsy in study patients while non-invasive tools are more commonly used to define fibrosis stage. Ultimately, there were only 37 hepatic decompensation events and 9 cases of HCC during the 8,210 person-years of follow-up, so confidence intervals around study estimates are quite wide.
My Practice
When I (SP) see a new patient for nonalcoholic fatty liver disease (usually seen on some imaging tests), one of my priorities as a hepatologist is to risk stratify their liver disease, i.e do they have fibrosis. I do this with the use of transient elastography (TE), which is commonly referred to as FibroScan, and which uses shear wave imaging to estimate liver stiffness.
TE can accurately diagnose cirrhosis and is useful in determining advanced fibrosis (F3/F4) from minimal or no fibrosis.5 If TE is unavailable, a FIB-4 index (that uses platelet count, ALT, AST, and age; online calculator https://www.mdcalc.com/fibrosis-4-fib-4-index-liver-fibrosis) that has good predictive
accuracy for advanced fibrosis.6 Should the TE or FIB-4 index be elevated or indeterminate, then MR elastography can be used, which examines the entire liver and can determine both fibrosis and fat fractions. However, it is not available everywhere and in those cases a liver biopsy may be warranted. Liver biopsy may also be done if the patient’s liver tests are elevated to help differentiate nonalcoholic steatohepatitis (NASH) from other liver diseases (such as autoimmune hepatitis, depending on serological markers).
If the patient is at low risk (TE < 8 kPa or FIB-4 index < 1.3), it is reasonable to continue to encourage dietary changes and weight loss with repeat testing in 2-3 years (if everything has remained stable). Those at indeterminate (TE 8-12 kPa, Fib-4 1.3-2.67) or high risk (TE > 12 kPa, FIB-4 > 2.67, or liver biopsy with F2-F4) would benefit from more intensive and structured weight loss programs, weight management medications, or bariatric surgery with close hepatology follow up.4
For Future Research
Larger cohorts followed for longer durations are still neededto provide precise prognostic data. Future studies of NAFLD therapies will need to demonstrate that regression from stage F3 fibrosis to stage F1-F2 translates into reduced risk of hepatic decompensation events.
Conflicts of Interest
The authors have no potential conflicts of interest.
REFERENCES
REFERENCES
1. Garcia-Tsao G. Nonalcoholic Steatohepatitis-Opportunities and Challenges. N Engl J Med 2021; 385; 17: 1615-17.
2. cotter TG, Rinella M. NAFLD 2020: The State of the Disease. Gastroenterology 2020; 158(7): 1851-54.
3. von Elm E, Altman DG, Egger M, et al. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med 2007; 147: 573-7.
4. Kanwal F, Shubrook JH, Adams LA, et al.. Clinical Care Pathway for the Risk Stratification and Management of Patients With Nonalcoholic Fatty Liver Disease. Gastroenterology. 2021;161(5):1657-1669.
5. Castéra L, Vergniol J, Foucher J, Le Bail B, Chanteloup E, Haaser M, Darriet M, Couzigou P, De Lédinghen V. Prospective comparison of transient elastography, Fibrotest, APRI, and liver biopsy for the assessment of fibrosis in chronic hepatitis C. Gastroenterology. 2005 Feb;128(2):343-50.
6. Shah AG, Lydecker A, Murray K, Tetri BN, Contos MJ, Sanyal AJ; Nash Clinical Research Network. Comparison of noninvasive markers of fibrosis in patients with nonalcoholic fatty liver disease. Clin Gastroenterol Hepatol. 2009 Oct;7(10):1104-12.

