Bariatric Surgery Is Superior to Lifestyle Changes + Best Medical Care for Metabolic Dysfunction-Associated Steatohepatitis: The BRAVES Study
 Yichin Fu, MD1 and Sonali Paul, MD, MS2
Yichin Fu, MD1 and Sonali Paul, MD, MS2
1Gastroenterology Fellow, University of Chicago School of Medicine, Chicago, IL
2Assistant Professor of Medicine, Division of Gastroenterology, Hepatology & Nutrition, Pritzker School of Medicine, the University of Chicago, Chicago, IL
This summary reviews Verrastro O, Panunzi S, Castagneto-Gissey L, et al. Bariatric-metabolic surgery versus lifestyle intervention plus best medical care in non-alcoholic steatohepatitis (BRAVES): a multicentre, open-label, randomised trial. Lancet 2023;401(10390):1786-1797.
Access the article through PubMed
Correspondence to Sonali Paul, MD, MS. Associate Editor. Email: EBGI@gi.org
STRUCTURED ABSTRACT Question: Does bariatric surgery (Roux-en-Y gastric bypass [RYGB] or sleeve gastrectomy) result in histologic resolution of metabolic-dysfunction associated steatohepatitis (MASH; previously known as nonalcoholic steatohepatitis [NASH]1) compared to lifestyle modification plus best medical care (i.e., Vitamin E supplements plus pioglitazone and liraglutide 1.8 g daily if patient had type 2 diabetes mellitus [DM])?
Design: Open-label trial randomizing participants to RYGB, sleeve gastrectomy, or lifestyle modification plus best medical care for 52 weeks. All patients received lifestyle modification counseling on diet and exercise.
Setting: Three centers in Rome, Italy.
Patients: Individuals aged 25-70 years of age with obesity (body mass index [BMI] 30-55 kg/m) with or without type 2 DM and histologically confirmed metabolic-dysfunction associated steatohepatitis. Key exclusion criteria included hemoglobin A1c ≥10%, significant cardiac comorbidity and familial dyslipidemia.
Exposure/Intervention: Eligible patients were randomized 1:1:1 to RYGB vs sleeve gastrectomy vs optimal medical care. All patients in the study received lifestyle modification counseling, defined as counseling to improve adherence to a diet containing two-thirds of the calorie expenditure per day, 10,000 steps per day, and 2-3 hours of moderate-intensity physical activity per week. In the best medical care arm, participants received vitamin E 800 IU/day plus pioglitazone and liraglutide 1.8 g daily if they also had type 2 DM since these agents have demonstrated positive effects on MASH. Surgical participants did not receive pharmacotherapy.
Outcome: The primary endpoint was histological MASH resolution without worsening of fibrosis at week 52. The main secondary outcome was improvement by at least 1 stage of the MASH fibrosis score with no worsening of MASH.
Data Analysis: Both intention-to-treat (ITT) and per-protocol analyses were reported.
Funding: The participating hospitals (Fondazione Policlinico Universitario A Gemelli, Policlinico Universitario Umberto I and S Camillo Hospital, Rome, Italy) funded the study.
Results: Overall, 288 adults with histologically confirmed MASH were included in the study and 236 (67%) completed the trial. Participants were 100% White, 44% women, mean age 47 years old, 32% with diabetes, mean body weight of 87.31 kg, BMI 41.8. While 88% of participants had stage F1 or 2 fibrosis, 11% (n=32) had F3 fibrosis. In ITT analysis, 56% and 57% of participants achieved resolution of MASH without worsening fibrosis with RYGB and sleeve gastrectomy, respectively, compared to 16% achieving resolution with lifestyle modification with best medical care (P<0.0001 for all comparisons among all 3 groups) (Figure 1a). Participants in the RYGB group and the sleeve gastrectomy group had 3.60 times (95% confidence interval [CI] 2.19–5.92; P<0.0001) and 3.67 times higher (2.23–6.02; P<0.0001) calculated probability of MASH resolution compared with the lifestyle modification plus best medical care group. Similar results were found in the per protocol analysis. Mean weight loss at 52 weeks was superior with RYBG and sleeve gastrectomy versus lifestyle modification plus best medical care: 31.8% vs 24.0% vs 5.5%, respectively (P< 0.0001).
In the ITT analysis, 37%, 39% and 23% of participants had improvement of fibrosis by at least 1 stage without worsening of MASH in the RYGB, sleeve gastrectomy, and lifestyle modification with best medical care, respectively (P=0.034) (Figure 1b). Nine percent of the RYGB group and 12% of the sleeve gastrectomy group had regression to Stage 0 fibrosis compared to 3% with lifestyle modification (P=0.0003).
Significantly more participants in the bariatric surgery groups had remission of their diabetes and improvement in liver biochemistries. There was no death or life-threatening complications, and 6% of the participants had severe adverse events but did not require re-operations.
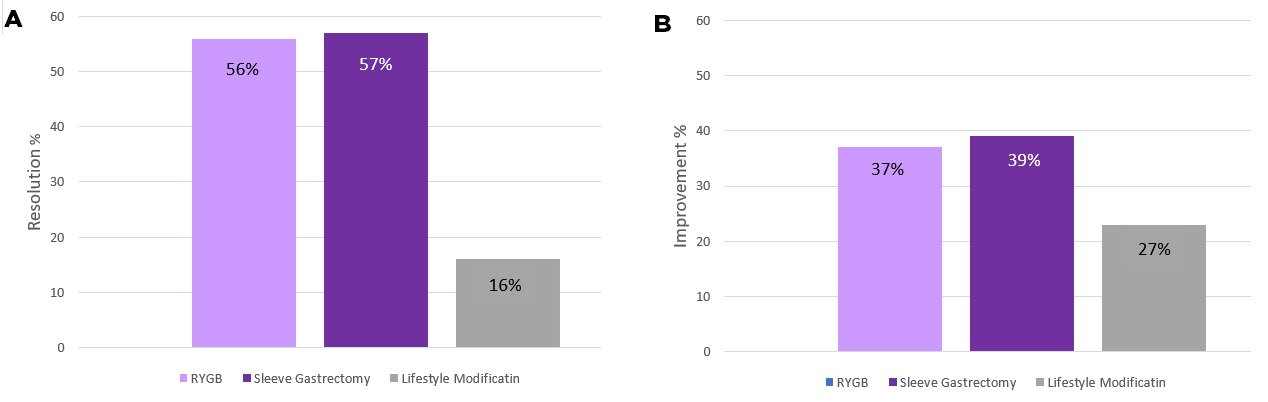 Figure 1. Resolution of MASH without worsening of fibrosis (A) and improvement of at least one stage of fibrosis without worsening of MASH (B).
Figure 1. Resolution of MASH without worsening of fibrosis (A) and improvement of at least one stage of fibrosis without worsening of MASH (B).Abbreviations: ITT, intention-to-treat; MASH, metabolic-dysfunction associated steatohepatitis; NASH, non-alcoholic steatohepatitis.
COMMENTARY
Why Is This Important?
Metabolic dysfunction-associated steatotic liver disease (MASLD; previously known as nonalcoholic fatty liver liver disease [NAFLD]1) is a growing public health concern globally, affecting not only liver health, but also cardiovascular mortality, and is quickly becoming the leading indication for liver transplantation. By 2030, approximately 30 million Americans will have MASH and approximately 5% will develop cirrhosis. Although no pharmacologic therapy is approved by the US Food and Drug Administration for the treatment of MASLD or MASH, weight loss is beneficial, with 3% weight loss reversing steatosis and 10% reversing fibrosis. Historically, bariatric surgery has had the most efficacious weight loss compared to pharmacotherapy, resulting in 25% to 30% weight reduction at 1-2 years. Patients with MASH and MASLD are often told about lifestyle interventions, with infrequent success. This randomized controlled trial is the first to demonstrate the benefits of bariatric surgery not only for weight loss, but also on MASH and fibrosis reversal, which are the ultimate goals of MASH treatment.
Bariatric surgery (RYGB or sleeve gastrectomy) is more effective than lifestyle modifications with best medical care (i.e., Vitamin E supplements plus pioglitazone and liraglutide for type 2 DM) for resolution of MASH and improvement in MASH fibrosis score.
Caution
While the results of this study are very promising, we need to be thoughtful of who we send to bariatric surgery for the treatment of MASH. First, the results may not be entirely generalizable to our patients, as the participants were all White and in Italy, where lifestyles are certainly different from the US. Also, best medical care patients with diabetes were given pioglitazone, which is not often used in clinical practice, and liraglutide 1.8mg daily. While liraglutide can be effective for weight loss, a higher dose (3.0 mg) is needed. Additionally, newer pharmacotherapies which can achieve >20% reduction in body weight, including semaglutide and tirzepatide,2-3 were not studied. Ongoing trials are investigating their efficacy for MASH.4 These weight loss therapies remain an option for individuals with MASH and obesity, especially if they also have type 2 DM. However, it remains unknown if newer pharmacotherapies can achieve similar weight loss as bariatric surgery.
My Practice
BMI > 35 or presence of metabolic disease with a BMI > 30 are indications for bariatric surgery. MASLD is a metabolic disease, but coverage based on MASLD alone is variable depending on insurance plan. However, most patients with MASLD have obesity, diabetes, or other components of metabolic syndrome. With the introduction of semaglutide and tirzepatide (off-label use) for weight loss into my practice, I try and use pharmacotherapy first before bariatric surgery. However, insurance often dictates medication coverage, making it not available to many patients. In those cases, bariatric surgery is considered. Insurance coverage is also variable for endoscopic sleeve gastrectomy. Whether surgery or pharmacotherapy, each is paired with important lifestyle interventions and counseling from a registered dietician. I am cautious in those with compensated cirrhosis given the risk of hepatic decompensation, but it could be done in select compensated patients.
For Future Research
In addition to better data across all racial/ethnic groups, more patients with F3 fibrosis need to be studied (there were only 11% in this study). Comparing efficacy of the newer anti-obesity medications to bariatric surgery in both the treatment of obesity and MASLD is also needed.
Conflicts of Interest
The authors have no reported conflicts of interest.
REFERENCES
- Rinella ME, Lazarus JV, Ratziu V, et al. A multi-society Delphi consensus statement on new fatty liver disease nomenclature [published online ahead of print, 2023 Jun 24]. Hepatology 2023;10.1097/HEP.0000000000000520.
- Jastreboff AM, Aronne LJ, Ahmad NN, et al. Tirzepatide once weekly for the treatment of obesity. N Engl J Med 2022;387(3):205–216.
- Wilding JPH, Batterham RL, Calanna S, et al. Once-weekly semaglutide in adults with overweight or obesity. N Engl J Med 2021; 384: 989-1002.
- Hartman ML, Sanyal AJ, Loomba R, et al. Effects of novel dual GIP and GLP-1 receptor agonist tirzepatide on biomarkers of nonalcoholic steatohepatitis in patients with type 2 diabetes. Diabetes Care 2020;43(6):1352-1355.

