Can IV Metoclopramide Improve Endoscopic Visualization for Patients with Active Upper Gastrointestinal Bleeding?
 Jeffrey Lee, MD, MPH
Jeffrey Lee, MD, MPH
Research Scientist and Attending Gastroenterologist, Kaiser Permanente San Francisco Medical Center, San Francisco, CA
This summary reviews Vimonsuntirungsri T, Thungsuk R, Nopjaroonsri P, et al. The efficacy of metoclopramide for gastric visualization by endoscopy in patients with active upper gastrointestinal bleeding: double-blind randomized controlled trial. Am J Gastroenterol 2024;119(5):846-855.
Access the article through The American Journal of Gastroenterology
Correspondence to Jeffrey Lee, MD, MPH. Associate Editor. Email: EBGI@gi.org
Keywords: metoclopramide, upper GI bleed, RCT, endoscopy
STRUCTURED ABSTRACT
Question: What is the efficacy of metoclopramide compared to placebo for gastric visualization in patients with active upper gastrointestinal bleeding (UGIB)?
Design: Double-blind, placebo-controlled randomized controlled trial (RCT).
Setting: Two medical centers in Thailand: the King Chulalongkorn Memorial Hospital, Sawanpracharak Hospital.
Patients: Adults ≥ 18 years with active UGIB (defined as having fresh or bright red blood within 24 hours or fresh blood during gastric lavage) who arrived in the emergency department and had an upper endoscopy within 12 hours after arrival. Adults were excluded if they had known prior gastric or duodenal surgery; known esophageal, gastric, or duodenal cancer; advanced HIV; and pregnant.
Interventions: Metoclopramide 10 mg administered intravenously between 30 to 120 minutes before the upper endoscopy. The comparison group was normal saline.
Outcomes: The primary outcome was the percentage of patients with adequate visualization in the metoclopramide group compared with the placebo group as determined by the Frossard scoring method. Secondary outcomes were the mean difference in endoscopic visualized gastroduodenal scores (EVS), duration of esophagogastroduodenoscopy (EGD), immediate hemostasis, the need for a second look EGD within 72 hours after initial endoscopy, unit of blood transfusion, length of hospital stay, and 30-day rebleeding rate.
Data Analysis: Intention-to-treat analysis. In addition, logistic regression was used to estimate the impact of treatment on adequate visualization.
Funding: The Gastroenterological Association of Thailand (GAT).
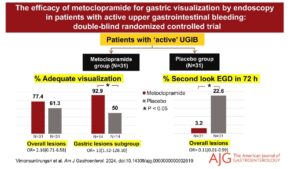
Results: Sixty-two patients (31 metoclopramide and 31 placebo) were enrolled and analyzed (Figure 1). The percentage of patients with adequate visualization was higher in the metoclopramide group versus in the placebo group (77.4% vs 61.6%, respectively; odds ratio [OR] 2.16 [0.71-6.58], P=0.16) but was not statistically significant. However, in gastric lesion subgroup analysis, metoclopramide improved the adequate visualization rate compared to placebo (92.9% vs 50%; OR 13.0 [1.32-128.10], P=0.03) and improved endoscopic visualization at the fundus. Lastly, metoclopramide reduced the need for second look EGD within 72 hours compared to placebo (3.2% vs 22.6%; OR -0.11 [0.01-0.99], P=0.02).
Figure 1. Visual abstract showing results.
COMMENTARY
Why Is This Important?
Acute upper gastrointestinal bleed (UGIB) is a common problem worldwide and is associated with significant morbidity and mortality.1 Endoscopy and its therapeutic interventions have been shown to reduce both rebleeding rates and mortality rates associated with acute UGIB.2 However, the effectiveness of endoscopic interventions for an UGIB is dependent on the quality of endoscopic visualization, which can be hampered by the presence of blood, clots, or other residues in the stomach and duodenum. Although current guidelines, including those pubished by the American College of Gastroenterology and European Society of Gastrointestinal Endoscopy,2,3 suggest the use of intravenous (IV) erythromcyin before endoscopy for an acute UGIB, it can prolong the QT interval, which can be associated with ventricular tachyarrhythmias and Torsade de Points. Thus, identifying a prokinetic agent that has rapid onset, easily accessible, and is safe and effective is urgently needed for the management of acute UGIBs. Therefore, this RCT from Vimonsuntirungsri and colleagues addresses this gap by evaluating the use of metoclopramide for gastric visualization during endoscopy in patients with acute UGIB.4
Key Study Findings
Metoclopramide did not provide much clinical benefit in terms of EGD duration, immediate hemostasis success rate, length of hospital stay, and 30 day rebleeding rate.
Caution
There are some limitations worth noting from this trial. First, the metoclopramide group had a lower hemoglobin level compared to placebo, suggesting a higher volume of blood loss in this group, which may have impacted the results. Second, metoclopramide improved visualization in the stomach from gastric lesions and reduced the need for a second look endoscopy within 72 hours; however, this trial was not adequately powered to evaluate these outcomes. Lastly, the study was conducted in 2 hospitals in Thailand, which limits the generalizability.
My Practice
I typically use prokinetic agents, either IV erythromycin 250 mg or IV metoclopramide 10 mg, for selected individuals with evidence of active upper GI bleeding or blood in the stomach such as hematemesis, coffee ground emesis, or a bloody nasogastric aspirate. The hope is that these prokinetic agents can help improve gastric visualization at the time of endoscopy by clearing the stomach of blood, clots, and food residue. I typically order these prokinetic agents to be administered intravenously 30 to 60 minutes prior to endoscopy. In determining which prokinetic agent to use, it’s mainly dependent on what is available at our medical center. However, most of the times, I’m mainly using erythromycin based on a meta-analysis of nearly 600 patients and 8 studies suggesting that giving erythromycin prior to the EGD results in decreasing the need for repeat EGD because of improved visualization.5 With the results from Vimonsuntirungsri et al.,4 there is now additional evidence, albeit from subgroup analyses, to support metoclopramide use prior to endoscopy for an acute UGIB, especially if I suspect the bleeding source is from the stomach. In addition to prokinetic agents, I will occasionally reposition the patient from the standard left later decubitus position to the left lateral “semi-recumbent” position with the head of the bed raised. This approach can also help clear blood, clots, or debris in the fundus.
For Future Research
Future studies should compare the effectiveness between metoclopramide versus erythromycin for improving gastric visualization among patients with acute active upper GI bleeding.
Conflict of Interest
Dr. Lee reports no potential conflict of interest.
REFERENCES
- Esrailian E, Ian M, Gralnek IM. Nonvariceal upper gastrointestinal bleeding: epidemiology and diagnosis. Gastroenterol Clin N Am 2005,34: 589-605.
- Laine L, Barkun AN, Saltzman JR, et al. ACG Clinical Guidelines: upper gastrointestinal and ulcer bleeding. Am J Gastroenterol 2021;116(5):899-917.
- Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic diagnosis and management of nonvariceal upper gastrointestinal hemorrhage (NVUGIH): European Society of Gastrointestinal Endoscopy (ESGE) Guideline – Update 2021. Endoscopy 2021;53(3):300-332.
- Vimonsuntirungsri T, Thungsuk R, Nopjaroonsri P, et al. The efficacy of metoclopramide for gastric visualization by endoscopy in patients with active upper gastrointestinal bleeding: double-blind randomized controlled trial. Am J Gastroenterol 2024;119(5):846-855.
- Rahman R, Nguyen DL, Sohail U, et al. Pre-endoscopic erythromycin administration in upper gastrointestinal bleeding: an updated meta-analysis and systematic review. Ann Gastroenterol 2016;29(3):312-7.