Kiwifruit-A Specific Food to Improve Stool Frequency in Patients With Mild Constipation

Philip Schoenfeld, MD, MSEd, MSc (Epi)
Chief (Emeritus), Gastroenterology Section, John D. Dingell VA Medical Center, Detroit, MI.
This summary reviews Gearry R, Fukudo S, Barbara G, et al. Consumption of 2 Green Kiwifruits Daily Improves Constipation and Abdominal Comfort-Results of an International Multicenter Randomized Controlled Trial. Am J Gastroenterol 2023; 118: 1058-68.
Access the article through PubMed
Correspondence to Philip Schoenfeld, MD, MSEd, MSc. Editor-in-Chief. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Do 2 green kiwifruit (without skin) per day significantly increase complete spontaneous bowel movements in patients with mild functional constipation or irritable bowel syndrome with constipation (IBS-C)?
Design: This is a multicenter, randomized cross-over trial comparing kiwifruit and psyllium. After a 2-week screening period to establish baseline symptoms, study participants were randomized to eat 2 green kiwifruits or to consume 7.5 grams of psyllium for 4 weeks. After an additional 4-week washout period, each patient crossed-over and completed a 4-week trial of the other treatment (Figure 1).
Setting: New Zealand, Japan, and Italy from 2014-2017.
Patients: Patients meeting Rome III criteria at initial screening for functional constipation (FC) (n = 60), IBS-C (n =61), and healthy controls (n=63).
Interventions/Exposure: Two green kiwifruits, without skin, vs 7.5 grams of psyllium husk daily. Two green kiwifruits and 7.5 grams of psyllium both contain approximately 6 gm of dietary fiber. It is important to note that approximately 2 teaspoons of brand name psyllium can contain approximately 6-7 mg of psyllium and 5 gm of dietary fiber.
Outcome: Primary endpoint was number of complete spontaneous bowel movements (CSBMs) per week. Although a specific definition of CSBM was not reported, it’s frequently defined as a spontaneous bowel movement with a complete sense of evacuation, which may or may not require absence of straining, too. Key secondary endpoints included gastrointestinal (GI) comfort based on GI Symptom Rating Scale (GSRS), stool consistency based on Bristol stool scale, and straining severity.
Data Analysis: Sample size was calculated to detect a CSBM increase of 1.5 per week in each constipated group (FC and IBS-C) compared to baseline. Intention-to-treat analyses were performed. Categorical endpoints were assessed with Chi-square test and continuous variables were assessed with a mixed models approach to repeated measures of analysis of variance. A hierarchical approach was used to deal with multiple secondary endpoints.
Funding: Zespri International, the world’s largest marketer of kiwifruit.
Results: In the combined FC/IBS-C group, study patients were primarily female (82%), European (60%) with mean age = 39 +/-15 and mean body mass index (BMI) = 23 +/- 4. Although the study did not specifically report baseline CSBM, the combined FC/IBS-C group appeared to have almost 4 CSBMs per week at baseline (Figure 2). Patients with FC increased their mean CSBMs per week with kiwifruit (1.53) and psyllium (0.67). In IBS-C patients, mean CSBMs per week increased with kiwifruit (1.73) and psyllium (1.25). When evaluating the combined FC/IBS-C group, kiwifruit produced significantly higher increases in mean CSBMs/ week vs psyllium (1.69 vs 0.90, P = 0.038) (Figure 2). Total GSRS scores were significantly lower after kiwifruit compared to psyllium in the combined FC/IBS-C group.
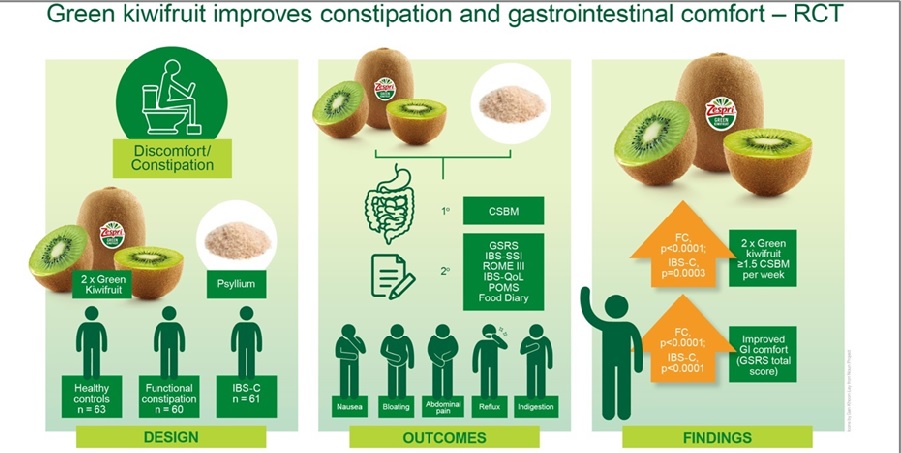
Figure 1. Randomized controlled trial design and results.
Abbreviations: CSBM, complete spontaneous bowel movement; FC, functional constipation; GI, gastrointestinal; GSRS, gastrointestinal symptom rating scale; IBS-C, irritable bowel syndrome with constipation; IBS-QoL, irritable bowel syndrome quality of life; IBS-SSI, irritable bowel syndrome with supplemental security income.
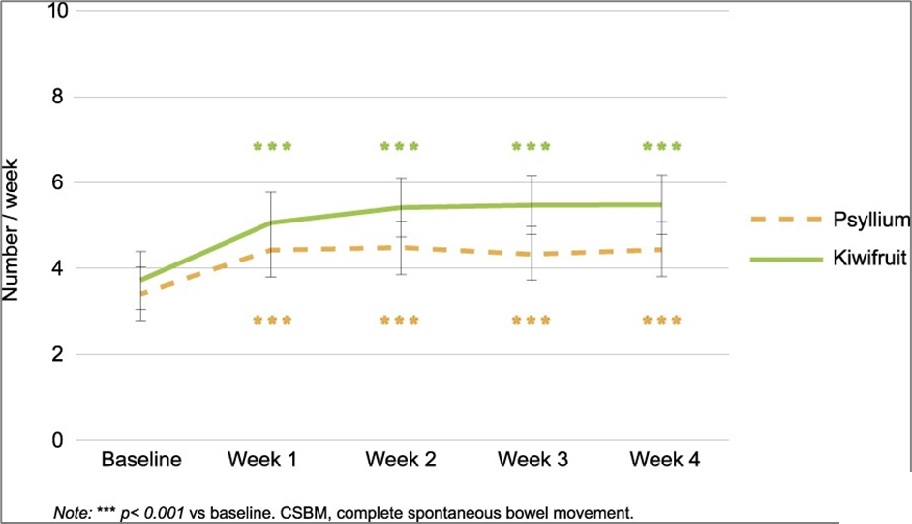
Figure 2. increase in complete spontaneous bowel movements from baseline in combined constipation (functional constipation + irritable bowel syndrome with constipation) patients. Abbreviations: CSBM, complete spontaneous bowel movement; FC, functional constipation; GI, gastrointestinal; GSRS, gastrointestinal symptom rating scale; IBS-C, irritable bowel syndrome with constipation; IBS-QoL, irritable bowel syndrome quality of life; IBS-SSI, irritable bowel syndrome with supplemental security income.
COMMENTARY
Why Is This Important?
Although we have multiple over-the-counter (OTC) and prescription therapies for chronic idiopathic constipation (CIC) with demonstrated efficacy1, many patients prefer dietary interventions. Simply suggesting that patients increase their dietary fiber may be too vague and unhelpful for patients, especially since “bran” fiber has not demonstrated efficacy in randomized controlled trials (RCTs).1 Prior to this research, prunes (or dried plums) contain sorbitol, act as osmotic laxatives, and were the only other specific food that demonstrated efficacy for increasing bowel movements.2-3 However, since prunes contain sorbitol and are high FODMAP foods, they may also increase bloating and worsen IBS symptoms. Kiwifruits provide an attractive alternative because their cell walls have a particularly pronounced swelling and water-holding capacity in vitro. This facilitates water retention in the lumen of the colon and could improve stool frequency and consistency.
Although this study has important limitations in design (see Caution section below), 2 green kiwifruit without skin appears to be effective for increasing CSBMs and this is at least the second RCT to demonstrate this.4 Therefore, this is an important advance for our patients.
When evaluating the combined group of patients with functional constipation or IBS-C, kiwifruit produced significantly higher increases in mean CSBMs/ week vs psyllium (1.69 vs 0.90, P = 0.038) (Figure 2).
Caution
Although patients met Rome III criteria for functional constipation or IBS-C at the onset of the initial 2-week lead-in/screening period, study patients appear to have had > 3 CSBMs/week when first randomized to kiwifruit or psyllium (Figure 2). This suggests that patients had very mild symptoms at onset of the trial, limits generalizability, and contrasts with the moderate-severe CIC patients with < 1 CSBM/week that have been enrolled in RCTs of constipation therapies. Also, the study duration is quite short for a chronic condition: 4 weeks in each treatment arm, and patients were unblinded about their treatment.
My Practice
Many of my patients dislike the consistency of psyllium/fiber supplements and desire dietary interventions. For these patients, prunes and kiwifruit are good recommendations, although prunes may increase bloating since it contains sorbitol. I also educate my patients that excessive consumption of water is unlikely to improve constipation symptoms unless it’s combined with an agent (e.g., kiwifruit) that facilitates water retention in the colon.
Per my previous commentary1, the vast majority of my patients have already tried and failed multiple OTC agents, including fiber supplementation, polyethylene glycol (PEG), or stimulant laxatives, prior to my evaluation. Although it’s certainly reasonable to discuss dietary modification for constipated patients, we should focus on asking patients what they have tried and failed in the past and then focus on initiating prescription therapies for moderate-severe symptomatic patients that make it to a gastroenterologist. Of course, shared decision-making is also critical. We must offer treatments that the patient will utilize and can afford. Unfortunately, many of my patients live in inner-city “food deserts” where they have limited access to well-stocked grocery stores with kiwifruit. Finally, don’t forget the basics when patients present for evaluation of chronic constipation. Do a digital rectal exam and assess for pelvic floor dysfunction/inappropriate ascent of the pelvic floor when the patient does a Valsalva maneuver. When I suspect pelvic floor dysfunction, especially in women who have had complicated vaginal deliveries and have failed multiple CIC therapies, I’ll order anorectal manometry and defecography.
For Future Research
Longer and better designed clinical trials would be helpful, although these studies would be expensive to conduct.
Conflict of Interest
Dr. Schoenfeld reports serving on advisory boards, consultant and speakers bureau for Ironwood Pharmaceuticals, AbbVie Pharmaceuticals, and Ardelyx Pharmaceuticals, and serving as an advisory board member for Salix Pharmaceuticals.
REFERENCES
- Schoenfeld P. AGA-ACG Clinical Practice Guideline on Chronic Idiopathic Constipation Treatments: Parsing Benefits and Risks. Evidence-Based GI July 2023. https://gi.org/journals-publications/schoenfeld_july2023/. Accessed August 10, 2023.
- Attaluri A, Donahoe R, Valestin J, Brown K, Rao SS. Randomised clinical trial: dried plum (prunes) vs psyllium for constipation. Aliment Pharmacol Therap 2011; 33: 822-28.
- Koyama T, Nagata N, Nishiura K, et al. Prune Juice Containing Sorbitol, Pectin, and Polyphenol Ameliorates Subjective Complaints and Hard Feces While Normalizing Stool in Chronic Constipation: A Randomized Placebo-Controlled Trial. Am J Gastroenterol 2022; 117: 1714-17.
- Chey SW, Chey WD, Jackson K, Eswaran S. Exploratory Comparative Effectiveness Trial of Green Kiwifruit, Psyllium, or Prunes in US Patients with Chronic Constipation. Am J Gastroenterol 2021; 116: 1304-12.

