The Pursuit of Excellence in Colonoscopy: Audit and Feedback Improves Polyp Detection in Low-Performers
Philip Okafor, MD, MPH1 and Uri Ladabaum, MD, MSc2
1Senior Associate Consultant, Department of Gastroenterology, Mayo Clinic, Jacksonville, Florida
2Professor of Medicine and Senior Vice-Chief, Division of Gastroenterology and Hepatology, Stanford University School of Medicine, Stanford, California
This article reviews Tinmouth J, Sutradhar R, Li Q, et al. A Pragmatic Randomized Controlled Trial of an Endoscopist Audit and Feedback Report for Colonoscopy. Am J Gastroenterol 2021; 116: 2042-51. https://doi.org/10.14309/ajg.0000000000001498 PMID: 34515669
Correspondence to Philip Okafor, MD, MPH Associate Editor. Email: EBGI@gi.org
performance?
the post-report period in both groups. The increase was not significantly higher in A&F group vs control group. (Table 1) However, among lowerperforming endoscopists with PR <25%, there was significantly more improvement in polypectomy rate for the A&F arm (17.9% to 23.8%) vs controls (19.4% to 23.3%) [RR: 1.34 vs 1.11, P=0.02]. Among low-performing endoscopists, mean ADR also improved more in the A&F group vs controls, though the difference was not significant (RR: 1.12 vs. 1.04, P=0.12). No differences were found in A&F effectiveness by specialty or annual colonoscopy volume. No significant differences were found in any secondary endpoints.
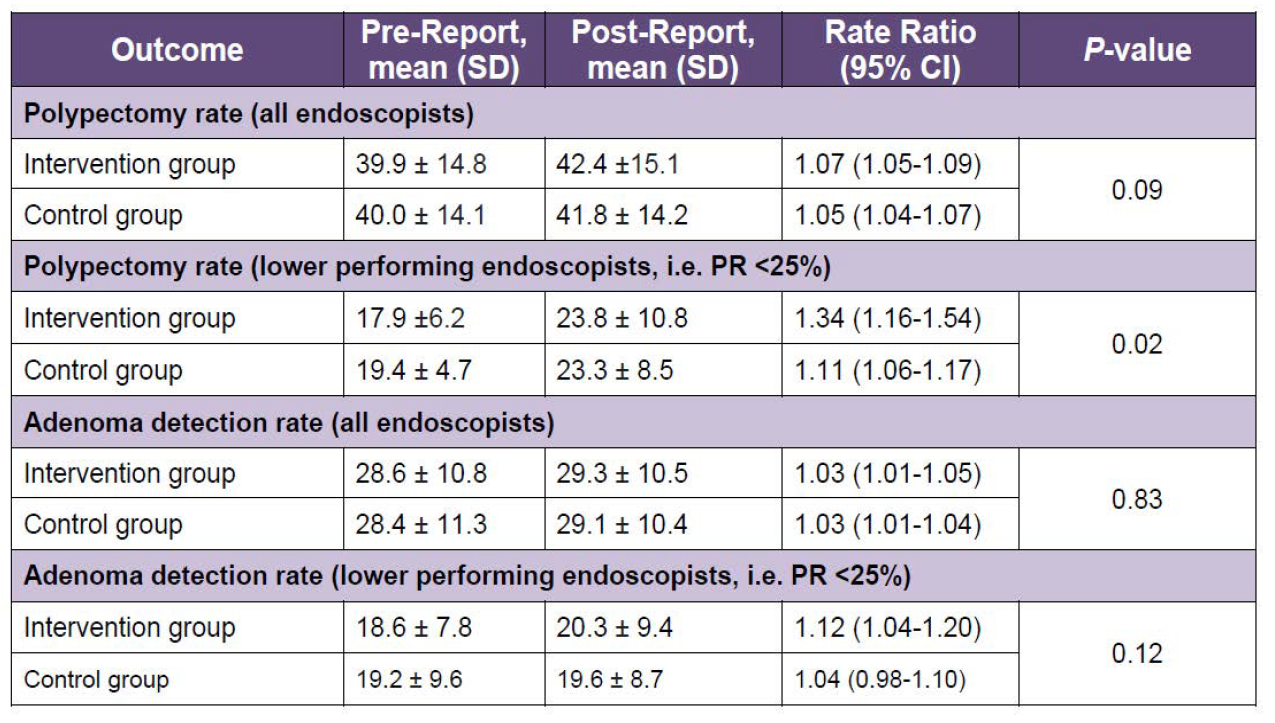
Table 1. Study Results. Mean PR showed no significant increase in audit and feedback group vs
the control group. CI, confidence interval; PR, polypectomy rate; SD, standard deviation.
_____________________________________________________________________
COMMENTARY
Why Is This Important?
The ADR has become one of the most widely used and validated quality measures and key performance indicators for screening colonoscopies.,sup>1 Despite its widespread recognition and the inverse association with interval colorectal cancer risk, there still exists significant variation in ADR among endoscopists.2
Research into endoscopist characteristics and their impact on ADR have yielded mixed results. For instance, a recent study showed no significant differences in ADR based on endoscopist’s specialty, sex, location of medical school, practice setting or presence of trainee during colonoscopy.3 As such, interventions to enhance ADR such as the optimization of withdrawal times, adoption of artificial intelligence, and utilization of technology-assisted colonoscopy are gaining traction.4
With current national ADR benchmarks set at greater than or equal to 25%, the need for sustainable interventions to improve this quality metric, particularly in low-performing endoscopists, has become essential. While artificial intelligence and technology-assisted colonoscopy sound promising, they are yet to reach primetime, underscoring the need for cheap, pragmatic, and scalable interventions. A&F have been shown to improve provider performance and this study by Tinmouth et al. provides evidence that it may also improve polyp detection among endoscopists with low ADRs.
Key Study Findings
Among low-performing endoscopists (i.e., endoscopists with polypectomy rate <25%), A&F led to a statistically greater improvement in polypectomy rate compared to control. A similar improvement was observed among all- endoscopists, but this did not meet statistical significance. Adenoma detection rates also improved but this was not statistically different between the intervention and control arms, though the study might have been underpowered to detect this difference.
Caution
This study provides some evidence that endoscopy performance can be improved with A&F, however, the sustainability of any impact particularly in the longterm, has not been reliably demonstrated. In addition, the authors in this study measured PR and ADR across all indications for colonoscopy, and not specifically for screening colonoscopies. As such, factors like case-mix and indication for the procedure could impact results. It is also essential to highlight that the impact of A&F on ADR was studied as a subgroup analysis and thus might have lacked the necessary power needed to detect a true change in ADR.
My Practice
Our institution (Division of Gastroenterology, Stanford University) has developed a reliable and easy mechanism to collect polyp data not just for ADR, but also serrated lesion detection rates (SLDR), advanced adenomas detection rate (AADR), and advanced serrated lesion detection rate (ASLDR) across the entire gastroenterology division over the past 7 years. This has relied on the buy-in of all endoscopists as the integrity of data collection relies heavily on the input of the group. This effort has grown to become collaborative and every quarter each endoscopist receives an email summary of their colonoscopy performance including data on the extent of exam, Boston Bowel Prep Score, withdrawal time, and indication for the colonoscopy. These data are collected for screening colonoscopies, surveillance colonoscopies, and diagnostic colonoscopies (performed for positive fecal immunochemical or multi-target stool DNA tests). Endoscopist data is compared to department averages for ADR, AADR, SLDR, and ASLDR.
We also receive feedback based on our consistency of providing surveillance recommendations to the referring provider. The ability to historically compare my performance with that of my peers has served as an internal drive that motivates me to consistently monitor the integrity and duration of my withdrawal. Personally, I (PO) use a counter on the screen in the endoscopy suite to ensure that an adequate amount of time is spent in each colonoscopy segment. Over time, this has led to my ADR improvement, which now approaches the highest in the division.
The main distinguishing features between our program and the A&F intervention tested by Tinmouth et al. are the socialization efforts and the frequency and context of feedback. We have been able to develop, institute and sustain our processes as a group, with multiple touch points at faculty meetings and individualized communications. This was not feasible in the province-wide effort by Tinmouth et al. This probably makes a big difference.
Our experience over the past 7 years, though anecdotal, suggests that the improvement from A&F in the context of a group effort to build a culture focused on high-quality care can lead to behavior changes, but we still maintain that the sustainability of any increase in colonoscopy key performance indicators from A&F needs to be studied in a prospective and rigorous manner.
For Future Research
This randomized control trial by Tinmouth et al. was adequately powered to demonstrate the impact of A&F on polyp detection. However, the impact on ADR was studied post hoc. Further studies that are powered to investigate the impact of A&F on ADR specifically (and AADR, SLDR, ASLDR) would provide needed high-quality evidence because some endoscopists can have a high polyp detection rate but have lower rates of detecting predominantly right-sided lesions such as serrated and advanced serrated lesions. There will also soon be a need for comparative effectiveness studies investigating the impact of technology-assisted colonoscopy versus or in combination with A&F on colonoscopy key performance indicators while quantifying the risk reduction on interval colorectal cancers.
Conflicts of Interest
The authors report no potential conflicts of interest.
REFERENCES
Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Am J Gastroenterol 2015;110:72-90.
2. Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370:1298-306.
3. Sarvepalli S, Garber A, Rothberg MB, et al. Association of Adenoma and Proximal Sessile Serrated Polyp Detection Rates With Endoscopist Characteristics. JAMA Surg 2019;154:627-635.
4. Brand EC, Wallace MB. Strategies to Increase Adenoma Detection Rates. Curr
Treat Options Gastroenterol 2017;15:184-212.

