Non-Erosive GERD Does Not Lead to an Increased Risk of Esophageal Adenocarcinoma: A Nordic Population Based Cohort Study
 Swathi Eluri, MD, MSCR
Swathi Eluri, MD, MSCR
Senior Associate Consultant, Mayo Clinic Florida, Jacksonville, FL; and Adjunct Assistant Professor of Medicine, University of North Carolina School of Medicine, Chapel Hill, NC
This summary reviews Holmberg D, Giola S, von Euler-Chelpin M, et al. Non-erosive gastro-oesophageal reflux disease and incidence of oesophageal adenocarcinoma in three Nordic countries: population based cohort study. BMJ 2023;382:e076017.
Access the article through PubMed
Correspondence to Swathi Eluri, MD, MSCR, Associate Editor. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Are patients with non-erosive gastroesophageal reflux disease (GERD) at an increased risk of developing esophageal adenocarcinoma?
Design: This is a population-based cohort study.
Setting: Hospitalized and specialized outpatient healthcare settings in Denmark, Finland, and Sweden.
Patients: Study included 486,556 adults (>18 years of age) with GERD who underwent upper endoscopy between January 1, 1987, to December 31, 2019. Of this group, 285,811 had non-erosive GERD and 200,745 in the validation cohort had erosive GERD. In the non-erosive GERD group, median interquartile range (IQR) age was 59 (44-70) years and 59% were women. In the erosive GERD group, median (IQR) age was 58 (45-69) years and 45% were women.
Exposure: Non-erosive GERD was defined by an absence of esophagitis and any other esophageal findings at endoscopy. Erosive GERD was defined by the presence of esophagitis at endoscopy.
Outcome: The incidence rate of esophageal adenocarcinoma was assessed for up to 31 years of follow-up.
Data Analysis: Standardized incidence ratios (SIR) with 95% confidence intervals (CI) of esophageal adenocarcinoma were calculated in the non-erosive GERD, erosive GERD groups, and the general population. Changes in standardized incidence ratios were assessed across 5 periods of follow-up: <1 year, 1-4 years, 5-9 years, 10-14 years, and 15-31 years, and plotted using Poisson regression. Stratified analyses were performed based on age, sex, and calendar period.
Funding: Swedish Research Council (2019-00209), Swedish Cancer Society (180684), and Nordic Cancer Union (186058).
Results: Among 285,811 patients with non-erosive GERD, the incidence rate of esophageal adenocarcinoma was 11 out of 100,000 person-years and was similar to that of the general population (SIR = 1.04; 95% CI: 0.91-1.18) and did not increase with longer (15-31 years) follow-up time (SIR = 1.07; 95% CI: 0.65-1.65). Those with erosive GERD were found to have 2.3 times the expected number of cancers compared to the general population (SIR = 2.36; 95% CI: 2.17-2.57) with increasing risk of progression to esophageal adenocarcinoma with longer follow-up time (SIR = 2.73; 95% CI: 2.15-3.42) (Figure 1).
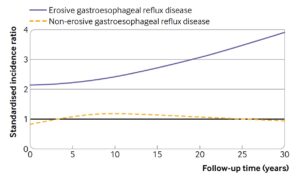
Figure 1. Standardized incidence ratios of oesophageal adenocarcinoma over follow-up time among patients with non-erosive (dashed line) and erosive (solid line) gastrooesophageal reflux disease compared with the general population of the same age, sex, and calendar period. Reproduced from article with permission from BMJ Publishing Group Ltd.
COMMENTARY
Why Is This Important?
GERD is a prevalent chronic condition, which when untreated can lead to complications such as erosive esophagitis, Barrett’s esophagus, and esophageal adenocarcinoma.1 However, a significant portion of patients with GERD do not develop erosive disease and subsequent clinical sequelae. Prior studies2 have investigated the risk of developing erosive esophagitis in GERD patients with a normal baseline endoscopy with reported prevalence ranging from 4%-5%. However, no prior study has been able to definitively estimate the incidence of esophageal adenocarcinoma in patients with non-erosive GERD and compare that with healthy controls. In other words, is there an increased risk of esophageal adenocarcinoma in patients with endoscopically-confirmed non-erosive GERD. If they aren’t at increased risk, then that infers that additional surveillance EGD is not needed to look for Barrett’s esophagus. The authors of this paper aimed to answer this question though a Nordic population-based cohort study with a very large patient population followed for over 30 years.
Key Study Findings
Caution
Although this is a well-designed, population-based cohort study in Nordic countries, there are significant methodologic limitations. Firstly, the diagnosis of GERD for the study population was made through a single International Classification of Diseases diagnostic code, which is neither sensitive nor specific. While it is likely that the patients in the erosive disease group had definitive pathologic GERD, it is highly plausible that a significant proportion in the non-erosive GERD group did not have pathologic acid reflux disease and likely could have had functional heartburn (i.e., patient complains of GERD symptoms, but does not have abnormal esophageal acid exposure or physiologic acid reflux that is correlated with GERD symptoms). This is an important delineation as the risk for developing Barrett’s esophagus and esophageal adenocarcinoma is not a concern in those with functional heartburn. Second, another major limitation is the lack of clarity regarding use of proton-pump inhibitor (PPI) therapy, especially in the erosive GERD group. Multiple studies2,3 have shown that PPIs successfully treat erosive esophagitis. If the patients in the non-erosive group were maintained on PPI therapy, they are less likely to develop complications such as cancer. Similarly, if a disproportionate number of patients in the erosive group were not maintained on PPIs, they are more likely to develop complications. One way to address this would have been to adjust for the use of PPI therapy, which would have strengthened the methodology. Finally, there is concern for misclassification bias, with patients who initially had erosive disease that improved with PPI therapy labeled as non-erosive. While patients in the non-erosive group were advised to stop PPIs a few weeks before their EGD, adherence to this is unknown and it is also unclear whether the duration of stopping PPI was sufficient for the reactivation of erosive disease.
My Practice
This study addresses a gap in literature regarding the risk of developing esophageal adenocarcinoma in GERD patients without erosive disease. Ultimately, the results of this study support what we do clinically.4,5 Specifically, ACG guidelines do not recommend repeat screening upper endoscopies in GERD patients with non-erosive GERD. It also re-affirms that EGD in GERD patients should be performed when they are off PPI for 2-4 weeks in order to assess for erosive esophagitis.
In my practice, I think that the nuanced interplay between true pathologic acid reflux, use of PPI therapy, recurrent symptoms, and disease complications such as Barrett’s esophagus, and esophageal adenocarcinoma need to be considered when deciding on optimal management. In patients with suspected GERD and a normal endoscopy, reflux monitoring performed off PPI therapy is most effective to confirm a diagnosis of symptomatic acid reflux.5 This facilitates adequately optimizing treatment of non-erosive GERD patients from an acid suppressive standpoint, which will help prevent the development of esophagitis and associated disease sequelae.
For Future Research
An optimal future study to answer this specific question would be a prospective cohort with baseline GERD confirmed by pH monitoring and use of standardized PPI therapy protocols.
Conflict of Interest
None to report.
REFERENCES
- Savarino V, Marabotto E, Zentilin P, et al. Pathophysiology, diagnosis, and pharmacological treatment of gastro-esophageal reflux disease. Expert Rev Clin Pharmacol 2020;13(4):437–49.
- Bardhan KD, Royston C, Nayyar AK. Reflux rising! An essay on witnessing a disease in evolution. Dig Liver Dis 2006;38:-8.
- Pace F, Bollani S, Molteni P, Bianchi Porro G. Natural history of gastro-oesophageal reflux disease without oesophagitis (NERD)–a reappraisal 10 years on. Dig Liver Dis 2004;36:-5.
- Shaheen N, Falk G, Iyer P, et al. Diagnosis and management of Barrett’s esophagus: an updated ACG guideline. Am J Gastroenterol 2022; 117: 559-87.
- Katz P, Dunbar K, Schnoll-Sussman F, et al. ACG Clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol 2022; 117: 27-56.

