In Case You Missed It:
Surgery is Superior to Medical Therapy for PPI-refractory Heartburn in the “Right” Patients

Jennifer M. Kolb, MD, MS
Assistant Professor of Medicine, Division of Gastroenterology, Hepatology and Parenteral Nutrition, VA Greater Los Angeles Healthcare System, David Geffen School of Medicine at UCLA, Los Angeles, CA
This summary reviews Spechler SJ, Hunter JG, Jones KM, et al. Randomized Trial of Medical versus Surgical Treat-ment for Refractory Heartburn. N Engl J Med 2019;381:1513-1523.
Correspondence to Jennifer M. Kolb, MD, MS. Associate Editor. Email: EBGI@gi.org
*In Case You Missed It is a recurring series about landmark RCTs from the past 3 years which impact new clinical practice guidelines.
Access the article through PubMed
STRUCTURED ABSTRACT
Question: Is laparoscopic Nissen fundoplication superior to medical therapy with PPI plus baclofen for patients with proton pump inhibitor (PPI)-unresponsive heartburn secondary to reflux.
Design: Randomized controlled trial (RCT) with 3 arms stratified based on impedance pH testing.
Setting: Veterans Affairs (VA) gastroenterology clinics.
Patients: Three hundred sixty-six patients referred to GI clinic for PPI-refractory heartburn were screened for eligibility by completing the Gastroesophageal Re-flux Disease-Health Related Quality of Life (GERD-HRQL) questionnaire followed by a 2-week trial of omeprazole 20 mg twice daily (30 minutes before breakfast and 30 minutes before dinner) for 2 weeks followed by completing the GERD-HRQL again. The GERD-HRQL is a validated questionnaire that ranges from 0 to 50 with higher scores indicating worse symptoms. Patients whose GERD-HRQL decreased by < 50% underwent diagnostic evaluation including endoscopy with biopsy, esophageal manometry, and esophageal impedance-pH monitoring while continuing omeprazole 20 mg twice daily. Inclusion criteria were: (a) abnormal acid exposure time (pH<4 for >4.2% of 24 hours); (b) symptom association probability >95% based on impedance-pH monitoring; or, (c) both. This ensured enrolling patients with abnormal acid reflux despite PPI therapy as well as individuals with reflux hypersensitivity who report GERD symptoms during physiologic reflux episodes although they do not have abnormal esophageal acid exposure time. Exclusion criteria included severe reflux esophagitis, non-GERD endoscopic abnormalities, eosinophilic esophagitis, achalasia, or absent contractility.
Interventions/Exposure: Study patients were randomized to: 1) surgical treatment with laparoscopic Nissen fundoplication; 2) active medical treatment with omeprazole 20 mg twice daily plus baclofen up to 20 mg 3 times daily followed by desipramine up to 100 mg nightly if baclofen was ineffective; and, 3) control medical treatment with omeprazole 20mg twice daily plus placebo.
Outcome: The primary outcome was treatment success, defined as a decrease of 50% of more in the GERD-HRQL score at 1 year. In the surgery group, treatment failure was also defined as resuming medication for heartburn. Secondary outcomes were the frequency of non-GERD disorders, anxiety, and depression, although these outcomes were not reported in this publication.
Data Analysis: Intention-to-treat analysis was performed, and Fisher’s exact test was used for pairwise comparison of treatment success across the groups.
Funding: Department of Veterans Affairs Cooperative Studies Program.
Results: Between August 29, 2012 through December 2, 2015, 366 patients were screened for the study, but 288 patients were excluded because of symptom resolution after 2-week PPI twice daily trial (12%), non-GERD disorders (6%), function-al heartburn/negative symptom-associated profile with normal acid reflux (27%), incomplete testing and other reasons (34%), 78 patients were randomized to surgery (n = 27), active medical treatment (n = 25), or control medical treatment (n = 26). Treatment success was higher in the surgical group compared to the active medical treatment (67% vs 28%, P=0.007, RR 2.43; 95% CI: 1.20-4.71) or control medical treatment (67% vs 12%, P<0.001, RR 5.78; 95% CI: 1.93-17.31) but there was no significant difference between the active medical group vs control medical group (P=0.17) (Figure 1). There were 5 serious adverse events in the surgery group (among 4 patients), 4 in the active medical group (4 patients), and 5 in the control medical group (3 patients).
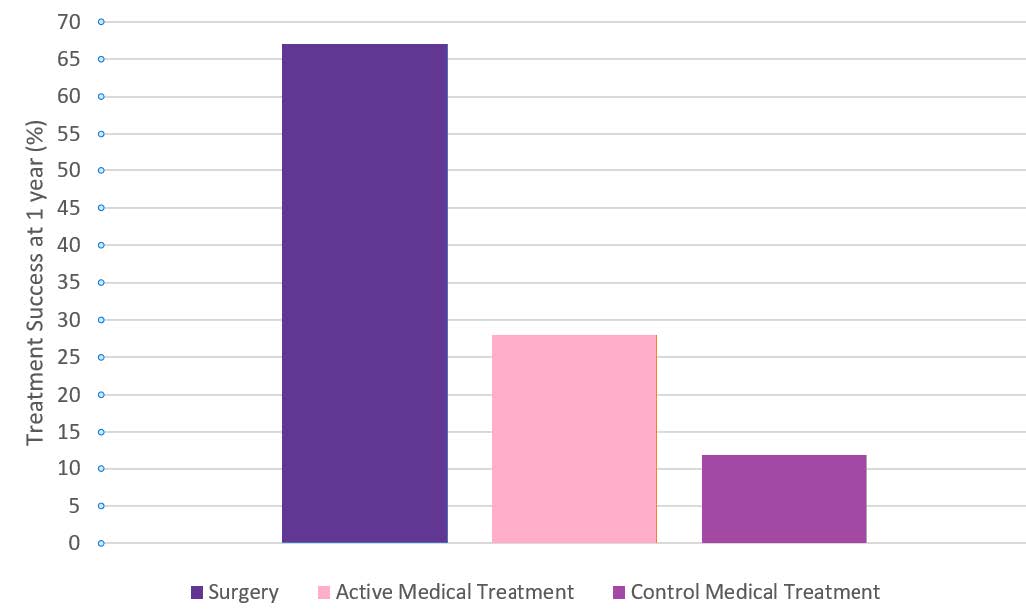
Figure 1: Treatment success at 1 year. Treatment success was defined as a decrease of 50% or more in the GERD-HRQL score from baseline. The incidence of treatment success with surgery was superior to active medical treatment (P = 0.007) or control medical treatment (P <0.001). The incidence of treatment success between the active medical group and the control medical group was 16% (P = 0.17).
COMMENTARY
Why Is This Important?
GERD affects almost 20% of the US population and causes significant bur-den and cost on the healthcare system. Heartburn is a challenging symptom that can negatively impact a person’s quality of life, interfere with everyday activities, and cause psychological dis-tress. PPIs are widely available over the counter so many people self-treat and they are also frequently prescribed by primary care doctors. Often, patients only reach gastroenterologists when their symptoms are not responding to medication. For PPI-unresponsive heartburn, the next steps in the workup should include upper endoscopy to evaluate for erosive esophagitis and/or manometry plus pH monitoring to confirm pathologic acid.1,2 If true PPI-unresponsive heartburn is confirmed, there is uncertain value in continuing the medication, and question of whether these individuals would respond to an anti-reflux procedure. This is the first study that evaluates medical versus surgical therapy in a pure cohort of PPI-unresponsive heartburn due to reflux. The rigorous pre-randomization evaluation was critical to identify those specific individuals.
The appropriate evaluation of PPI-refractory heartburn is particularly important because its common and has multiple etiologies. First, failure to properly take PPI twice daily (30 minutes before breakfast and dinner) is common and an easy fix. However, if patients are adherent, then simply switching PPIs or increasing dosage is frequently insufficient. After ruling out non-GERD disorders, including eosinophilic esophagitis, achalasia, other esophageal motility disorders, atypical chest pain due to cardiovascular disease, costochondritis, and even panic attacks, it’s important to rule out functional heartburn with impedance-pH monitoring (i.e., patients complaining of heartburn despite no abnormal esophageal acid exposure nor positive symptom-associated profile in response to physiologic reflux). These are not appropriate candidates for surgery.
The first important takeaway is that only 23% of patients referred to GI clinic for PPI-refractory heartburn actually had abnormal acid reflux and/or confirmed reflux symptoms based on pH-impedance monitoring while on twice daily omeprazole. During the pre-randomization phase, 12% of patients had a response to PPI, 6% had non-GERD disorders and 27% had functional heartburn.
In the highly selective group of individ-uals with heartburn that is PPI-refractory and due to reflux, laparoscopic Nissen fundoplication was more effective than medical therapy with twice daily omeprazole plus baclofen followed by desipramine.
Caution
This study was performed in a Veteran population which was largely White males, which could limit generalizability. More importantly, the updated trial protocol was not adequately powered to detect differences between active medical therapy with omeprazole, baclofen, and desipramine vs control medical treatment limited to omeprazole, although the trend favored active medical therapy.
My Practice
At any opportunity during a clinic visit or endoscopy, I ask patients when they are taking their PPI in relation to food and try to help them find a good schedule based on timing of their symptoms and their meals. Since 12% of study patients referred for PPI-refractory heart-burn had an adequate response to twice daily PPI taken 30 minutes before breakfast and dinner, this underscores the importance of providing clear instructions to the patient on how and when to take their medications to optimize efficacy. Switching to another PPI and/or increasing the dose may be helpful since polymorphisms of the hepatic CYP2C19 or CYP3A4 enzymes may impact the metabolism and duration of action of different PPIs. Esophageal motility disorders, non-esophageal diseases, and functional dis-orders can all result in heartburn and GERD-like symptoms, emphasizing the value of a comprehensive diagnostic workup. I typically perform an upper endoscopy with pH testing to confirm the diagnosis then tailor medications. H2 receptor blockers can be added for nocturnal symptoms, alginate antacids can be used for breakthrough symptoms, and baclofen for belching or regurgitation. Simple lifestyle interventions such as avoiding meals at night, elevating the head of the bed, avoiding trigger foods, weight loss if obesity is contributing, and smoking cessation can have a meaningful impact. If these interventions are inadequate and diagnostic work-up demonstrates abnormal acid reflux and/or confirmed reflux symptoms based on pH-impedance monitoring, then the updated ACG Clinical Guideline on the Diagnosis and Management of Gastroesophageal Reflux Disease recommends surgery for these patients, largely based on this RCT. Per the guideline, surgery is also an option for patients with LA Grade C/D erosive esophagitis despite PPI use and large hiatal hernias. This potential option should be brought up early so that patients can become more comfortable with this idea.
For Future Research
This well designed and supported study encountered numerous obstacles to patient enrollment since so few patients met inclusion criteria after diagnostic work-up, which led to intra-trial protocol amendments. This suggests that future studies may face similar challenges and alternative approaches are needed to evaluate GERD treatments.
Conflict of Interest
The author has no conflicts of interest.
REFERENCES
- Yadlapati R, Gyawali CP, Pandolfino JE, et al. AGA Clinical Practice Update on the Personalized Approach to the Evaluation and Management of GERD: Expert Review. Clin Gastroenterol Hepatol 2022; 20: 984-994.e1.
- Katz PO, Dunbar KB, Schnoll-Sussman FH, et al. ACG Clinical Guideline for the Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol 2022;117:27-56.
Download the article summary (PDF)

