In Case You Missed It
It’s (Usually) OK to Wait Until Morning to Scope that Patient with UGI Bleeding
Philip Schoenfeld, MD, MSEd, MSc (Epi)

Chief (Emeritus)-Gastroenterology Section, John D. Dingell VA Medical Center, Detroit, MI
______________________________________________________________________________________________________
This article reviews Lau JYW, Yu Y, Tang RSY, et al. Timing of Endoscopy for Acute Upper Gastrointestinal Bleeding. N Engl J Med 2020; 382: 1299-308. doi: 10.1056/NEJMoa1912484
Correspondence to Philip Schoenfeld, Editor-in-Chief. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Is urgent esophagogastroduodenoscopy (EGD) (within 6 hours of GI evaluation) superior to early EGD (within 24 hours of GI evaluation) for reducing all-cause mortality or further GI bleeding in high-risk patients with melena or hematemesis?
Design:Single-center, randomized controlled trial.
Setting: Prince of Wales Hospital, Shatin, Hong Kong. Investigators from Institute of Digestive Diseases, Chinese University of Hong Kong.
Patients: Inpatients with overt acute upper gastrointestinal bleeding (UGI; hematemesis, melena, or both) and high risk for death and/or further bleeding based on a Glasgow-Blatchford bleeding score of 12-23 were randomized. The Glasgow-Blatchford bleeding score is based on heart rate, systolic blood pressure, hemoglobin, blood urea nitrogen, presentation with melena or syncope, and presence of cardiac failure and/or hepatic disease and risk stratifies patients on need for blood transfusion and endoscopic intervention. All patients received appropriate initial resuscitation with intravenous fluids and/or transfusion plus IV proton pump inhibitors with 80mg bolus plus 8mg/hour continuous infusion. Patients in hypotensive shock despite resuscitation were excluded.
Exposure/Intervention: Urgent EGD within 6 hours of GI consultation vs early EGD within 24 hours of GI consultation. In the early EGD group, patients who had their initial GI consultation between 8 AM and 11:59 PM underwent endoscopy the following morning.
Outcome: The primary endpoint was 30-day all-cause mortality rate. Secondary endpoints included persistent bleeding at conclusion of index endoscopy or recurrent bleeding (e.g., recurrent hematemesis, melena after normalization of stool color, new tachycardia or systolic hypotension, hgb drop of 2g/dl after hgb stabilizataion, etc), use of hemostatic interventions (e.g., hemoclips, contact thermocoagulation, band ligation for varices) during index endoscopy, duration of hospitalization and intensive care unit stay, blood transfusions, need for surgery or angiographic embolization, need for further endoscopic hemostatic treatment, and 30-day adverse event rate.
Data Analysis: Intention-to-treat analysis. Investigators achieved complete follow-up of patients with no missing data. Log-rank test used to compare time from randomization to death and/or further bleeding. Cox proportional hazards used to estimate hazard ratios.
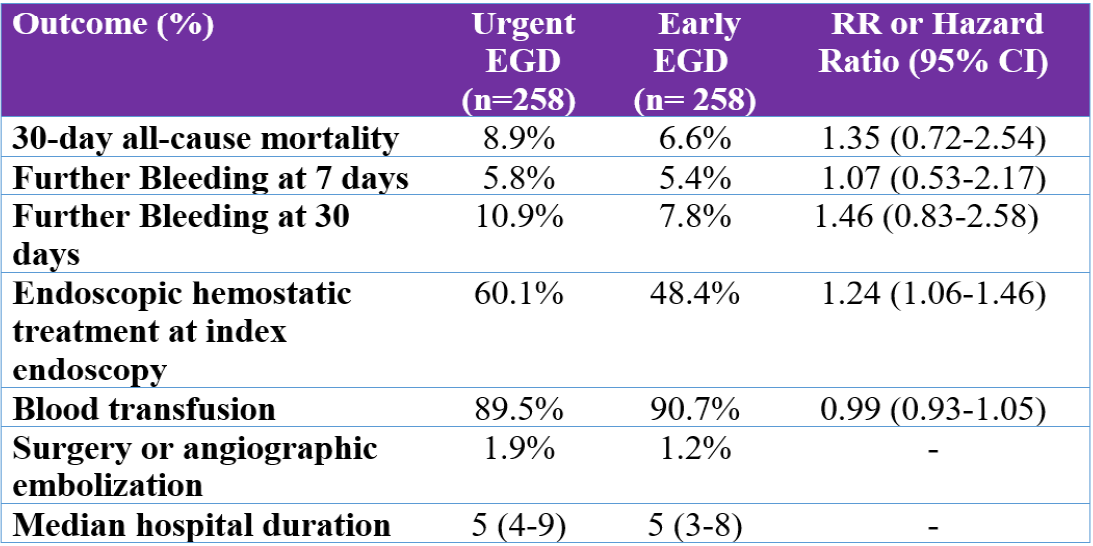
Results: There were 516 inpatients randomized (mean age: 70-71 years old; 63% male; average Glasgow-Blatchford bleeding score-13.7; 8.5% variceal bleed on index endoscopy; 61% peptic ulcer on index endoscopy). Due to a lag of approximately 8 hours between initial presentation with UGI bleeding (UGI) and GI consultation, this equated to patients getting EGD at means of 10 and 25 hours after presentation. There was no advantage for urgent EGD vs early EGD for any primary or secondary endpoint (Table 1), although endoscopic interventions were performed more commonly in the urgent-EGD group: 60.1% vs 48.4%; hazard ratio (HR)= 1.24 (95% confidence interval [CI]: 1.06-1.46). The study hypothesis was that urgent EGD would be beneficial. However, mortality rate and further bleeding rate were numerically lower in the early EGD group, although this was not a statistically significant difference.
Funding: The Health and Medical Fund of the Food and Health Bureau, Government of Hong Kong Special Administrative Region.
Table 1. 30-day all-cause mortality, further bleeding, and other secondary endpoints.
CI, confidence interval; EGD, esophagogastroduodenoscopy; RR, relative risk.
COMMENTARY
Why Is This Important?
Prior guidelines from the GI societies in the US, Europe, and Asia suggested that EGD within 12 hours should be considered in patients with UGI bleeding and hemodynamic instability at presentation in order to reduce mortality and further bleeding.1 However, observational studies provide conflicting results about potential benefits of urgent EGD. Also, urgent EGD within 6 hours of presentation could be detrimental if adequate hemodynamic stabilization with IV fluids and stabilization of other chronic medical conditions hasn’t been completed. Resolving this issue is crucial since acute UGI bleeding is the most common medical emergency faced by gastroenterologists. Thus, the landmark RCT conducted by Drs. Lau, Chan, Sung and their colleagues at the Chinese University of Hong Kong provides crucial data.
Their study results do not demonstrate any benefit for urgent EGD, especially among individuals with non-variceal UGI bleeding who can be stabilized hemodynamically. Primarily due to the results of this RCT, the 2021 ACG Clinical Guideline on Upper Gastrointestinal and Ulcer Bleeding2 eliminated the suggestion from the 2012 ACG guideline that EGD within 12 hours “may be considered” in high-risk patients. Instead, the 2021 ACG guideline authors emphasizes the importance of resuscitation with IV fluids and transfusion and stabilization of active co-morbid conditions before EGD is performed.
Key Study Findings
There was no advantage for urgent EGD vs early EGD for mortality or further UGI bleeding, which are the most important endpoints in this type of trial. Although endoscopic therapeutic interventions were performed more commonly in the urgent EGD group: 60.1% vs 48.4%; HR = 1.24 (95% CI: 1.06-1.46), this did not translate into a reduction in further UGI bleeding, which was numerically lower in the early EGD group.
Caution
This is a remarkably well-designed study with few limitations. Considering that about 8.5% (44/516) of study patients had esophageal or gastric varices and the natural history of acute esophageal variceal bleeding differs from peptic ulcer bleeding, these data may not be applicable to patients with a history of variceal bleeding or known cirrhotics. Also, this study excluded patients who had persistent “hypotensive shock” despite resuscitation attempts.
My Practice
My practice essentially mirrors the treatment of early EGD patients from this randomized controlled trial, which is also consistent with the conditional recommendation from the ACG Clinical Guideline on UGI and Ulcer Bleeding.2 When a patient presents with melena or hematemesis plus tachycardia/systolic hypotension, then resuscitation with intravenous fluids and blood transfusion (threshold of hemoglobin < 7) to achieve hemodynamic stability is emphasized, regardless of time of day when I’m consulted. After hemodynamic stability is achieved, then EGD is performed within 24 hours of presentation. As per this RCT’s “early-EGD” protocol, this usually means that EGD is performed around 8 AM on morning after presentation.
I’ll perform EGD urgently if the patient doesn’t become hemodynamically stable after appropriate resuscitation. If a patient has a history of esophageal variceal bleeding, then I may perform EGD sooner while still emphasizing cardiovascular resuscitation with intravenous fluids along with IV octreotide and IV ceftriaxone for presumed variceal bleed.
For Future Research
Data from well-designed randomized controlled trials about the efficacy of urgent endoscopy (within 6-12 hours) for patients with cirrhosis, past history of variceal bleeding, or persistent hypotensive shock despite resuscitation is lacking.
Conflict of Interest
Dr. Schoenfeld reports no conflicts of interest.
References
1. Laine L. Timing of Endoscopy in Patients Hospitalized with Upper Gastrointestinal Bleeding. N Engl J Med 2020; 382: 1361-62.
2. Laine L, Barkun A, Saltzman JR, et al. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am J Gastroenterol 2021; 116: 899-917.