Endoscopic Sleeve Gastroplasty Is Effective for Patients With Obesity Who MERIT Intervention
Jennifer M. Kolb MD, MS1 and Austin L. Chiang, MD, MPH2
1Assistant Professor of Medicine, Division of Gastroenterology, Hepatology and Parenteral Nutrition, VA Greater Los Angeles Healthcare System, David Geffen School of Medicine at UCLA, Los Angeles, CA
2Assistant Professor of Medicine, Division of Gastroenterology and Hepatology, Thomas Jefferson University Hospital, Sidney Kimmel Medical College of Thomas Jefferson University, Philadelphia, PA
This summary reviews Dayyeh BKA, Bazerbachi F, Vargas EJ, et al. Endoscopic sleeve gastroplasty for treatment of class 1 and 2 obesity (MERIT): a prospective, multicentre, randomised trial. Lancet 2022; 400: 441–51.
Access the article through PubMed
Correspondence to to Jennifer M. Kolb, MD, MS. Associate Editor. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Is endoscopic sleeve gastroplasty (ESG), a minimally invasive, endoluminal, organ-sparing bariatric procedure, safe and effective for patients with class 1 (body mass index [BMI] 30-<35 kg/m2) and class 2 obesity (BMI 35-<40 kg/m2)?
Design: Prospective, multicenter, unblinded, randomized clinical trial (RCT).
Setting: Nine academic and community centers (5 gastroenterology, 4 bariatric surgery) in the US.
Patients: Adult patients aged 21-65 years with BMI 30-40 kg/m2 who had previously failed non-surgical weight loss methods. Patients with a history of gastrointestinal surgery or gastrointestinal inflammatory disease were excluded.
Interventions/Exposure: Lifestyle modifications included a low-calorie diet plan and physical activity counseling customized to the individual. ESG was performed by experienced proceduralists who underwent a standardized training program with a commercially available, full-thickness endoscopic suturing device (OverStitch; Apollo Endosurgery, Austin, TX). Patients were randomly assigned in a 1:1.5 ratio using stratified permuted blocks to either the ESG group (ESG + moderate-intensity lifestyle modifications) or the control group (moderate-intensity lifestyle modifications alone). At 52 weeks, participants in the control group who did not reach the target weight loss goal were offered crossover to receive ESG and followed for another 52 weeks.
Outcomes: The primary outcome was excess weight loss (EWL) at 52 weeks with ESG compared to lifestyle intervention alone. EWL was calculated as: (weight loss from initial to follow up divided by baseline excess weight) x 100. Baseline excess weight was defined as index weight minus ideal weight based on BMI of 25 kg/m2. Durability was evaluated in the primary ESG group for a total of 104 weeks. Secondary efficacy endpoints at 52 weeks were proportion of patients with 25% or more EWL, 5% or 10% more of total body weight loss (TBWL), and percentage of TBWL. The effect of ESG on obesity comorbidities was also assessed. Safety endpoints were evaluated using the Clavien-Dindo grade, which is a standardized and validated system to define and grade post-surgical events based on the therapy needed to address the adverse event.
Data Analysis: Efficacy at 52 weeks was assessed on both a per-protocol basis (participants who completed the 52-week visit) and a modified intention-to-treat basis. The primary outcome (% EWL) was assessed using a linear mixed-effects regression model.
Funding: Mayo Clinic and Apollo Endosurgery (manufacturer of the OverStitch System) provided grant support to conduct research, but site investigators conducted the study and controlled data.
Results: Between December 20, 2017 and June 14, 2019, a total of 209 study patients (mean age 46-47; approximately 86% female; mean weight approximately 216 pounds/99kg) were randomly assigned to ESG (n=85) or control (n=124). The mean %EWL was 49.2% (SD 32.0) in the ESG group and lower at 3.2% (SD 18.6) in the control group (P <0.001). Similarly, TBWL at 52 weeks was higher with ESG compared to control (12.6% vs 0.8%, P <0.0001), which equates to approximately 27 pounds vs 2 pounds. On modified intention-to-treat analysis adjusted for age, sex, diabetes, hypertension, and BMI, participants in the ESG group had a mean difference of 44.7% EWL and 12.6% TBWL compared to the control group (Figure 1). For the secondary endpoint, 77% in the ESG group compared to 12% in control group achieved 25% or more EWL at 52 weeks. At 52 weeks, 9 patients in the ESG group did not meet the primary endpoint of 25% EWL and 5 of these underwent suture reinforcement. This consists of a repeat endoscopy with placement of additional sutures to shorten and tighten the stomach. Individuals who had crossover ESG achieved mean 44.1% EWL after 52 weeks, achieving similar success as the primary ESG group.
Among the 60 patients who had ESG and achieved >25% EWL, most (68%) maintained this at 104 weeks. Diabetes metrics (fasting glucose, hemoglobin A1C) and hypertension improved significantly in the ESG group but had minimal to negative change in the control group. There were 6 (4%) individuals who required hospital admission for medical management of expected post procedure accommodative gastrointestinal symptoms. There were 3 (2%) device-related or procedure-related adverse events including abscess managed endoscopically, upper GI bleed managed conservatively, and malnutrition requiring endoscopic sleeve reversal.
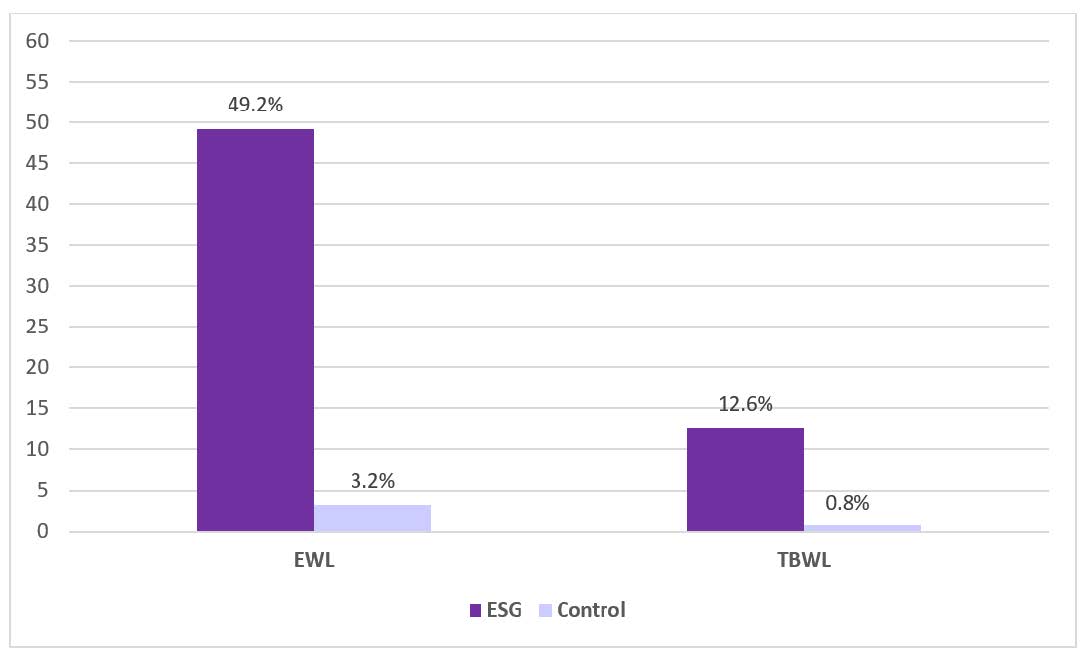 Figure 1. Primary outcome results. Percent of excess weight loss (EWL) and mean total body weight loss (TBWL) at week 52. ESG, endoscopic sleeve gastroplasty.
Figure 1. Primary outcome results. Percent of excess weight loss (EWL) and mean total body weight loss (TBWL) at week 52. ESG, endoscopic sleeve gastroplasty.COMMENTARY
Why Is This Important?
Obesity rates continue to rise in the United States affecting nearly half of individuals older than 20 years, of whom 10% meet criteria for severe obesity.1 Obesity is a chronic disease and significant contributor to major morbidities such as heart disease, stroke, diabetes, and cancer. Despite the growing utilization of bariatric surgery, it still has failed to reach even a fraction of patients who would benefit from an intervention. Endoscopic approaches are an alternative option for individuals who either do not qualify for bariatric surgery due to anatomy/prior surgeries or severe comorbidities or who do not want surgery due to potential complications. It can also be a bridge to bariatric surgery.
ESG utilizes full thickness suturing along the greater curvature to create a tubular stomach that mimics a surgical sleeve but preserves the fundus. ESG is mainly considered in patients with BMI of 30-40 kg/m2, but can be an option for individuals with a higher BMI >40 kg/m2 or BMI 27-30 with comorbid illness, especially if refractory to pharmacotherapy. It is performed using the OverStitch endoscopic suturing system which was FDA approved in July 2022 for ESG and endoscopic bariatric revision in patients with BMI 30-50 kg/m2. ESG has been performed worldwide and consistently demonstrated improvement in TBWL of 15%-20%. In a meta-analysis of 1,772 patients who had ESG, participants achieved a mean TBWL at 6, 12, and 18-24 months of 15.1%, 16.5%, and 17.2%.3 Five year durability data from Sharaiha et al showed a mean TBWL of 15.9%.4 ESG has also yielded improvements in metabolic parameters including hemoglobin A1c, liver enzymes, serum triglyceride, and systolic blood pressure.5
This study by Abu Dayyeh et al is the first randomized trial to demonstrate efficacy outcomes with ESG and life-style modifications compared to lifestyle changes alone for patients with obesity. Not only did patients achieve and maintain meaningful weight loss, but they also had marked improvement in their metabolic comorbidities. This landmark trial establishes ESG as the main player in our endoscopic obesity treatment armamentarium at the present time.
Key Study Findings
In this RCT of ESG with lifestyle interventions compared to lifestyle interventions alone, the ESG group had significantly greater and meaningful weight loss.
The ESG group also had improvement in their metabolic comorbidities. ESG was overall very safe with a 2% rate of device or procedure related serious adverse events. Durability of ESG was also demonstrated. Of the 60 patients who achieved their goal weight of >25% EWL at 1 year, 41 (68%) had sustained weight loss using the same definition at 2 years.
Caution
This study still does not answer the question of how ESG compares to laparoscopic sleeve gastrectomy. Future comparative studies will be useful to determine patient characteristics that may predict success and to help patients make informed decisions based on effectiveness and safety profile. Additionally, this trial only provides data out to 2 years and at the 1-year mark, suture reinforcement was offered. More robust long-term data will be important to show durability of ESG and guide practice on when a repeat endoscopy with tightening may be indicated.
My Practice:
I (JK) work with a multidisciplinary group that includes a bariatric surgeon, registered dietician, obesity medicine specialist, psychologist, health/behavior coach, and pharmacist. This team-based comprehensive approach is critical to implement a multitargeted intervention. In our Veteran’s Affairs setting, this is accomplished through the MOVE! weight loss program for veterans. Like the workup for bariatric surgery, potential candidates should undergo a thorough medical, psychological and lifestyle evaluation to ensure there are no other conditions that would interfere with their post procedure lifestyle and diet. Ideally these individuals have good functional status and can exercise. One of the most important keys to success is a motivated patient who is ready and willing to follow instructions and stay engaged with the team. Although I typically require patients to complete and “fail” a full lifestyle intervention program prior to consideration for ESG as they do for bariatric surgery, this article with a crossover design suggests that this approach is likely only causing a detrimental delay for patients without improved outcomes. These results also reinforce the limited success with lifestyle/diet alone and suggest we may need to be more aggressive up front with an endoscopic intervention, surgical intervention, or effective weight loss medications such as GLP-1 agonists. Indeed, for patients who do not achieve at least 5% TBWL in the first month after ESG or even show signs of weight regain, I add on weight loss pharmacotherapy to augment response.
For Future Research
ESG is becoming mainstream with more and more gastroenterologists and surgeons being trained daily. Its popularity is expected to continue to grow as insurance companies recognize its value and provide reimbursement. Alternative technologies for gastric remodeling procedures that are being evaluated are the primary obesity surgery endoluminal (POSE), which employs a similar concept as ESG but utilizes full thickness plications with suture anchor pairs. Additional weight loss interventions such as intragastric balloons, the transpyloric shuttle, and new techniques, including duodenal mucosal resurfacing and metabolic focused interventions, with different mechanisms of action are being developed as we learn more about the pathophysiology of obesity and concomitant metabolic disorders. Clearly, there are millions of Americans with obesity that cannot be reached through surgery alone. Refining algorithms for a comprehensive approach to obesity care will require collaboration from all members of the healthcare team, the institution and payors, industry partners, and researchers. Additionally, endoscopic therapies may play a larger role in the growing obesity epidemic in children and adolescents.
Conflict of Interest
Dr. Kolb reports no potential conflict of interest. Dr. Chiang is an employee of Medtronic.
REFERENCES
- 1. Hales CM CM, Fryar CD, Ogden CL. Prevalence of obesity and severe obesity among adults: United States, 2017–2018. NCHS Data Brief, no 360. Hyattsville, MD: National Center for Health Statistics, 2020.
- Camilleri M, Malhi H, Acosta A. Gastrointestinal Complications of Obesity. Gastroenterology 2017;152:1656-1670.
- Hedjoudje A, Abu Dayyeh BK, Cheskin LJ, et al. Efficacy and Safety of Endoscopic Sleeve Gastroplasty: A Systematic Review and Meta-Analysis. Clin Gastroenterol Hepatol 2020;18:1043-1053 e4.
- Sharaiha RZ, Hajifathalian K, Kumar R, et al. Five-Year Outcomes of Endoscopic Sleeve Gastroplasty for the Treatment of Obesity. Clin Gastroenterol Hepatol 2021;19:1051-1057 e2.
- Sharaiha RZ, Kumta NA, Saumoy M, et al. Endoscopic Sleeve Gastroplasty Significantly Reduces Body Mass Index and Metabolic Complications in Obese Patients. Clin Gastroenterol Hepatol 2017;15:504-510.
Download the Article Summary (PDF)



