In Case You Missed It
Peroral endoscopic myotomy (POEM) for Achalasia: At Least As Good As Laparoscopic Heller’s Myotomy
 Jennifer M. Kolb MD, MS1 and Kenneth J. Chang, MD2
Jennifer M. Kolb MD, MS1 and Kenneth J. Chang, MD2
1Assistant Professor of Medicine, Division of Gastroenterology, Hepatology and Parenteral Nutrition, VA Greater Los Angeles Healthcare System, David Geffen School of Medicine at UCLA, Los Angeles, California
2Professor and Chief, Gastroenterology and Hepatology, Executive Director, Digestive Health Institute, University of California, Irvine, California
This summary reviews: Werner YB, Hakanson B, Martinek J, et al. Endoscopic or Surgical Myotomy in Patients with Idiopathic Achalasia. N Engl J Med 2019;381:2219-2229.
Access the Article through PubMed
Correspondence to Jennifer M. Kolb, MD, MS, Associate Editor. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Is peroral endoscopic myotomy (POEM) as effective as surgical laparoscopic Heller’s myotomy (LHM) with Dor’s fundoplication for patients with idiopathic achalasia?
Design: Prospective, multicenter, unblinded, randomized non-inferiority clinical trial.
Setting: Eight centers in 6 European countries.
Patients: Adult patients with symptomatic achalasia (subtypes I, II, and III) confirmed on manometry and with Eckardt score >3 who had not undergone any prior esophagogastric surgery. Patients who had undergone prior endoscopic interventions such as pneumatic dilation or botox were allowed.
Interventions/Exposure: Patients were randomly assigned in a 1:1 ratio to POEM or LHM with Dor’s fundoplication, which were performed according to current standards by experienced endoscopists and surgeons
Outcome: The primary outcome was clinical success defined as Eckardt score <3 at 2-year follow-up. The Eckardt symptom score is a validated questionnaire that is calculated by grading 4 components: dysphagia, regurgitation, chest pain, and weight loss. Each component is graded on a 0-3 scale with higher scores indicating more severe symptoms. Secondary outcomes included symptoms (Gastrointestinal Quality of Life Index score and GERD), endoscopic findings of esophagitis, manometry, and abnormal acid exposure time on pH studies. Clinical data was collected as 3, 6, 12, and 24 months, and endoscopy, manometry, and esophageal pH studies were performed at 3 and 24 months
Data Analysis: Primary analysis was a modified intention-to-treat which included all patients randomized and the assigned intervention. Additional analyses included per-protocol population which was all patients in this modified intention-to-treat population who completed follow up.
Funding: European Clinical Research Infrastructure Network; Olympus Europa, and additional public foundations.
Results: Between December 7, 2012 and October 9, 2015, 221 study patients were enrolled and assigned to POEM (n=112) or LHM (n=109). At 2 years, clinical success, defined by Eckardt score < 3, was similar in POEM and LHM patients (83.0% vs 81.7%) and met predefined criteria for non-inferiority (difference = 1.4 percentage points, 95%CI -8.7 to 11.4, P=0.007 for non-inferiority). Clinical success rates were similar between groups at 3, 6, 12, and 24 months (Figure 1). Eleven patients had persistent symptoms: 2 of 3 in the POEM group had reintervention and all 8 patients in the LHM had reintervention. Improvement in esophageal function as measured by the integrated relaxation pressure of the lower esophageal sphincter on manometry was similar between the 2 groups (difference -.075 mm Hg, 95% CI -2.26 to 0.76). Improvement in symptoms according to the Gastrointestinal Quality of Life Index scores was also similar between the 2 groups (difference 0.14 points, 95% CI -4.01 to 4.28).
Reflux esophagitis on endoscopy was higher in the POEM group compared to LHM group, respectively, at 3 months (57% vs 20%, odds ratio [OR]= 5.74, 95% CI 2.99-11.00) and 24 months (44% vs 29%, OR = 2.00, 95% CI 1.03-2.85), although rates of LA Grade C/D erosive esophagitis were similar in both groups at 3 months (6% vs 3%) and 24 months (5% vs 6%). Proton-pump inhibitor (PPI) use was also more common in the POEM group vs LHM group at 24 months (52.8% vs 27.2%). Serious adverse events were numerically lower in POEM vs LHM groups (2.7% vs 7.3%) but this difference was not statistically significant.
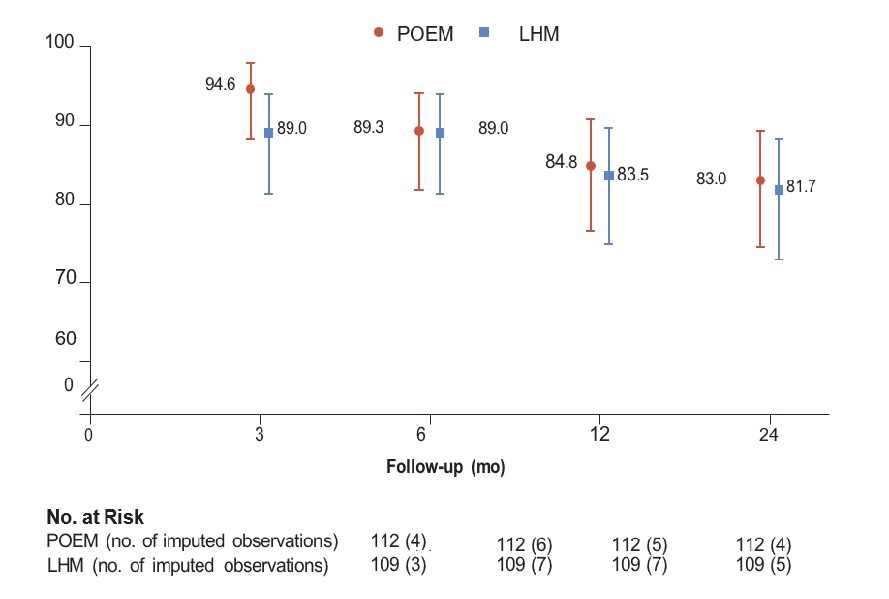
Figure 1: Percentage of Patients with Clinical Success
COMMENTARY
Why Is This Important?
Esophageal motility disorders are becoming more mainstream as our diagnostic modalities expand and our therapeutic armamentarium grows. Although the traditional approach to treating achalasia had always been LHM or pneumatic dilation, POEM has gained traction as a less invasive, safe, and effective option. A meta-analysis of 36 studies including 2,372 patients demonstrated high rates of clinical success (Eckardt score <3: 98%), with varying rates of symptomatic GERD (8.5%), erosive esophagitis on endoscopy (13%), and abnormal acid exposure (47%).1
This is the first randomized trial to directly compare POEM to LHM in patients with all subtypes of achalasia. Since this landmark article, multiple professional GI society guidelines have adopted POEM as a comparably effective first line therapy for patients with type I or type II achalasia and a preferred treatment option for those with type III achalasia.2-4 Further evidence for this change in practice comes from a recent study in JAMA Surgery that used insurance claims data to highlight a 19 fold increase in POEM utilization from 2010 to 2017.5
Key Study Findings
In a head-to-head comparison, clinical success was similar between POEM and LHM for patients with achalasia. Secondary outcomes including improvement in manometry and quality of life scores were also similar. Serious adverse events occurred in 2.7% of patients who had POEM and 7.3% who had LHM. GERD is common after both interventions and initially higher in patients who undergo POEM compared to LHM, but at 24 months the rates of LA Grade C/D esophagitis are similar. Correspondingly, POEM patients were more likely to be using PPIs at 2-year follow-up (52.8% vs 27.2%). This is not surprising since LHM patients also get an anti-reflux measure, the Dor fundoplication in this study.
Caution
Endoscopists in this study underwent formal POEM training and supervision, emphasizing that POEM is a highly technical procedure that requires specialized training. This study did not address the optimal therapy for patients who have had prior esophageal or stomach surgery or prior surgical therapy for achalasia.
My Practice
The combination of medical and surgical history, anatomy, and patient preference are critical factors in choosing the optimal therapy for achalasia. For type I (“classic” with minimal contractility in the esophageal body) and type II (with intermittent periods of panesophageal pressurization) achalasia, POEM and LHM are both effective options and I always offer patients a surgical consultation, but find that they prefer the endoscopic, less invasive approach. POEM is the first line therapy for type III achalasia (spastic with premature or spastic distal esophageal contractions), and we tailor the myotomy to the length of the spastic segment on manometry, esophagram, and Endoflip. Patients who have had prior esophageal surgery or LHM and need a redo myotomy are often best served by POEM due to the difficulty of repeat operation. Patients who are newly diagnosed with achalasia in a practice where POEM is not offered should be referred to a center where POEM is performed. As of January 2022, there is a CPT code for POEM so this is recognized and reimbursesd by insurance carriers and getting approval should not be an issue.
The Achilles heel remains post-POEM reflux and the possibility for significant silent GERD and catastrophic complications such as erosive esophagitis, Barrett’s esophagus, and even cancer. For my anti-reflux POEM, I use a modified posterior approach with a navigational tunnel method that allows for predictable navigation of the myotomy to finish at the lesser curve of the stomach and avoid disruption of the gastric sling fibers. We have adapted our technique to do a shorter myotomy on both the esophageal and cardia side. We are even moving towards only cutting the circular muscle rather than disrupting the longitudinal fibers (full thickness) as we learn more about the physiology of dysphagia and GERD. All patients come back at 3-6 months for endoscopic evaluation and esophageal pH testing. Patients with significant acid reflux who do not wish to continue lifelong medication may benefit from transoral incisionless fundoplication which recreates and lengthens the gastroesophageal flap valve.
For Future Research
The technique of POEM continues to be refined as we learn more about risk factors for post-POEM reflux. Further studies are needed to determine the indications and timing for antireflux interventions— whether at the same time as POEM analogous to a LHM with fundoplication or at a subsequent session. Another topic of ongoing investigation is determining the optimal therapy for non-achalasia spastic esophageal disorders and what role POEM plays in these conditions.
Conflict of Interest
Drs. Kolb and Chang reported no potential conflict of interest.
REFERENCES
- Akintoye E, Kumar N, Obaitan I, et al. Peroral Endoscopic Myotomy: A Meta-Analysis. Endoscopy 2016;48:1059-1068.
- Oude Nijhuis RAB, Zaninotto G, Roman S, et al. European Guidelines on Achalasia: United European Gastroenterology and European Society of Neurogastroenterology and Motility recommendations. United European Gastroenterol J 2020;8:13-33.
- Vaezi MF, Pandolfino JE, Yadlapati RH, et al. ACG Clinical Guidelines: Diagnosis and Management of Achalasia. Am J Gastroenterol 2020;115: 1393-1411.
- Khashab MA, Vela MF, Thosani N, et al. ASGE Guideline on the Management of Achalasia. Gastrointest Endosc 2020;91:213-227 e6.
- Lois AW, Oelschlager BK, Wright AS, et al. Use and Safety of Per-Oral Endoscopic Myotomy for Achalasia in the US. JAMA Surg 2022;157:490-497.

