Over-the-Scope Clips Decrease Non-Variceal Upper GI Bleeding vs Standard Endoscopic Treatment… In the Right Patient

Jennifer M. Kolb MD, MS
Assistant Professor of Medicine, Division of Gastroenterology, Hepatology and Parenteral Nutrition, VA Greater Los Angeles Healthcare System, David Geffen School of Medicine at UCLA, Los Angeles, CA
This summary reviews Lau JYW, Li R, Tan C et al. Comparison of Over-the-Scope Clips to Standard Endoscopic Treatment as the Initial Treatment in Patients With Bleeding From a Nonvariceal Upper Gastrointestinal Cause: A Randomized Controlled Trial. Ann Intern Med 2023 Apr;176(4):455-462. doi: 10.7326/M22-1783
Correspondence to Jennifer M. Kolb, MD, MS. Associate Editor. Email: EBGI@gi.org
Access the article through PubMed
STRUCTURED ABSTRACT
Question: Are over-the-scope clips (OTSC) more effective than standard endoscopic hemostatic treatments (hemoclips and/or contact thermocoagulation with or without pre-injection of diluted epinephrine) for nonvariceal upper gastrointestinal bleeding (NVUGIB) in patients with non-bleeding visible vessels (Forrest IIa) or actively bleeding ulcers (Forrest Ia/Ib)?
Design: Multicenter, unblinded, randomized controlled trial (RCT)
Setting: Seven university teaching hospitals in Hong Kong, China, and Australia. Approximately 58% of patients enrolled at Prince of Wales Hospital in Hong Kong.
Patients: Adult patients presenting with nonvariceal upper gastrointestinal bleeding were screened and recruited. Patients found to have active bleeding (pulsatile or Forrest Ia bleeding, oozing from a visible vessel or Forrest Ib bleeding), or a non-bleeding visible vessel (Forrest IIa) on endoscopy were randomized. If clot over bleeding lesion was observed, then irrigation and elevation of area was performed. If a vessel was then seen, the patient was randomized. Patients could be excluded if they were not believed to be OTSC candidates due to the position of NVUGIB lesion (e.g., pyloric channel).
Interventions/Exposure: Patients were randomly assigned at time of endoscopy in a 1:1 ratio to standard hemostatic treatment (hemoclips and/or contact thermocoagulation with heater probe or bipolar device +/- pre-injection of diluted epinephrine) or OTSC 11T (cap size 11mm; teeth with small spikes) (Figure 1) followed by 72 hours of intravenous proton pump inhibitor (PPI) therapy followed by oral PPI. All study investigators/endoscopists received at least 2 weeks of training at Prince of Wales Hospital on OTSC use, including bench deployment and case observation. Randomization was stratified into blocks of 10 by lesion and size (1-ulcer size <10mm, ulcer size 10mm-20mm, 3-ulcer size >20mm, 4- non ulcer lesion) at Prince of Wales Hospital. At the other sites randomization was not stratified. Salvage therapy with any tool was allowed if initial therapeutic attempt failed.
Outcome: The primary outcome was the 30-day probability of further bleeding, which was a composite endpoint of failure to control bleeding (primary hemostasis) and recurrent bleeding within 30 days. Recurrent bleeding was defined as fresh hematemesis, hematochezia, or melena associated with hypotension/tachycardia and/or drop of 20g/l of hemoglobin within 24 hours and endoscopic confirmation of fresh blood in the GI tract on urgent repeat endoscopy. Additional outcomes included failure of primary hemostasis, recurrent bleeding after initial hemostasis, need for further intervention (endoscopic, angiographic, surgical), need for blood transfusion or hospitalization, and 30-day mortality.
Data Analysis: Intention-to-treat analysis used to calculate time-to-event analysis and Kaplan-Meier curves.
Funding: University Grant Committee to the Government of the Hong Kong Special Administrative Region. They had no role in the design, conduct, or study analysis.
Results: Between January 2018 to December 2020, 706 patietnts were screened, 527 were consented, 191 were randomized and 190 were included for analysis (standard group n=97, oTSC n=93). In the overall cohort, mean age was 62-62 year, male 77%-80%, and endoscopic finding of peptic ulcer was 90%-92%. In the standard group, the most common hemostasis techniques were combined epinephrine injection plus hemoclips or thermocoagulation (n=51), hemoclips alone (n=26), or thermocoagulation alone (n=12). The cumulative 30-day probability of further bleeding was higher in the standard vs OTSC group: 14.6% vs 3.2%; risk difference: 11.4%, 95% confidence interval (CI): 3.3-20.0, P=0.006 (Figure 2). Failure at primary hemostasis was higher in the standard versus OTSC group (6.2% vs 1.1%; risk difference: 5.1, 95% CI: 0.7-11.8), while recurrent bleeding at 30 days was numerically higher in the standard vs OTSC group (8.8% vs. 2.2%, risk difference 6.6, 95% CI: -0.3 to 14.4). In the OTSC group, 1 death was related to ulcer perforation and pneumoperitoneum found at the time of readmission for femur fracture. There was 1 instance where an OTSC for an antral ulcer caused a pyloric obstruction and had to be removed.
 Figure 1: Type T over-the-scope-clip.
Figure 1: Type T over-the-scope-clip.
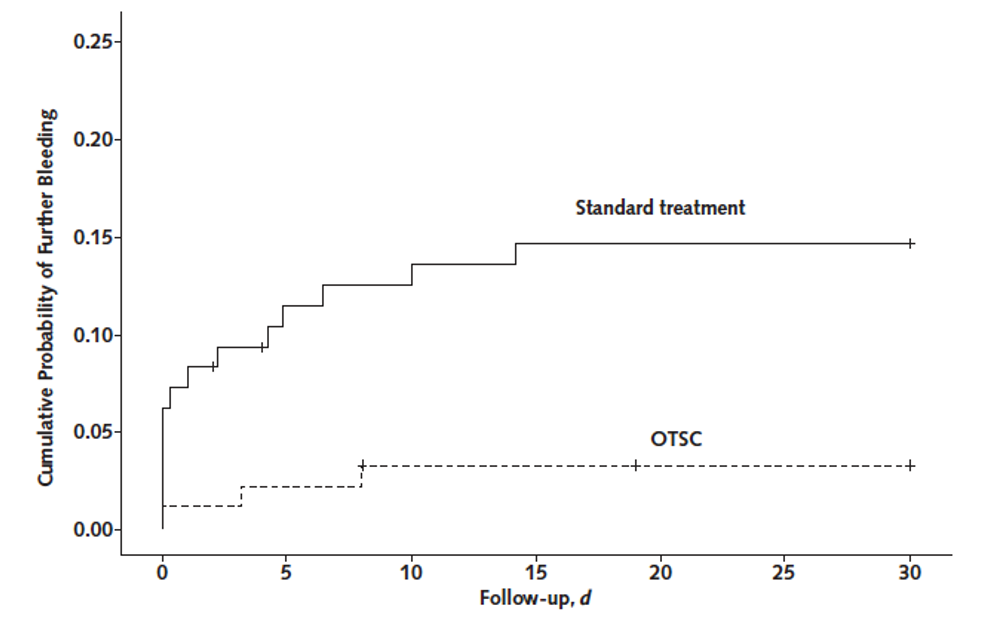
Figure 2: 30-day probability of further bleeding. Figure 2: 30-day probability of further bleeding.
COMMENTARY
Why Is This Important?
NVUGIB is a common reason for hospital admission and one of the most frequent consults to the GI service. The endoscopic approach to treating peptic ulcer disease with active bleeding or a visible vessel has remained largely unchanged for many years and includes the use of through the scope hemoclips or thermal therapy, with or without injection of diluted epinephrine, followed by 72 hours of intravenous PPI therapy.1-2 Nevertheless, primary hemostasis is not always achieved for actively bleeding ulcers and there is about 10%-20% risk of recurrent bleeding for high-risk lesions even when primary hemostasis is achieved with current endoscopic interventions.
OTSCs are a more recent addition to our armamentarium for the management of GI bleeding.3-4 These are large nitinol clips that are mounted on a clear plastic cap that is attached to the endoscope (Figure 1). The cap facilitates suction to bring in tissue, followed by deployment and closure of the large jaws or “bear claw” to compress the tissue, similar to the jaws closing on a hunting trap. These OTSCs are used for closure of perforations in the colon and upper gastrointestinal tract.5 RCTs assessing their efficacy for nonvariceal upper GI bleeding have generally demonstrated superiority of OTSCs to standard endoscopic intervention but had various methodologic limitations. Thus, current guidelines only recommend use of OTSCs for persistent or recurrent NVUGIB and their positioning in the algorithm for primary hemostasis needed to be clarified. This well-designed RCT on OTSC as first line therapy may change future guideline recommendations.
Key Study Findings
OTSC had better outcomes than standard hemostatic therapies across all categories.
Caution
As the study investigators acknowledge in the publication, inherent methodologic limitations of endoscopic research may bias results towards superiority of OTSC. The study excluded 10 patients with lesions “with endoscopic appearance or positions considered not favorable for OTSC placement,” such as duodenal ulcers where OTSC closure could lead to pyloric channel obstruction. There were also 3 patients randomized to the OTSC arm that were technically limited and OTSC could not be applied. Given prior data showing a benefit of OTSC for refractory bleeding, this trial design allowed for rescue OTSC if classic hemostatic approaches were not working, and this could have impacted endoscopists subjective assessment of successfully achieving primary hemostasis. Finally, OTSC use requires training, although it’s a relatively simple technique for skilled endoscopists to learn.
My Practice
I learned how to place OTSC during my fellowship training and routinely teach my GI fellows to use them. I often grab for these first when I see active bleeding or a high-risk lesion in the upper GI tract, such as ulcers with a visible vessel that are larger than 2 cm or located on the lesser curve of the stomach or if the ulcer is in gastroduodenal artery territory, such as the posterior duodenal bulb. I consider several other factors when deciding what hemostatic approach to use and keep in mind some limitations with OTSC. First, the clips work best when the vessel is clearly visualized straight ahead. It can be tricky to use these in certain parts of the duodenum if there is angulation or difficulty tipping the scope up. Once the clip is mounted on the scope, the cap can make visualization a bit more challenging, especially if there is active bleeding, so it is important to understand where the lesion is compared to surrounding structures. Injecting epinephrine prior to OTSC placement is an option to facilitate visualization by temporarily stopping bleeding. The tissue anchor is theoretically useful to grab and pull up a fibrotic ulcer base, though I have never needed this in clinical practice. If the patient has recently been on anticoagulation or needs to restart medication, I tend to prefer definitive treatment with OTSC and avoid thermal therapy. I also like using OTSC for dieulafoy lesions in the stomach since these submucosal arteries can be deeply penetrating and OTSC offers deeper, more secure hemostasis.
For Future Research
Future studies should evaluate predictors of rebleeding in acute NVUGIB treated with OTSCs and standard therapy to define algorithms for future use. These should incorporate elements of cost effectiveness.
Conflict of Interest
Dr. Kolb reports no potential conflict of interest.
REFERENCES
- Laine L, Barkun AN, Saltzman JR, et al. ACG Clinical Guideline: Upper Gastrointestinal and Ulcer Bleeding. Am J Gastroenterol 2021; 116: 899-917.
- Gralnek IM, Stanley AJ, Morris AJ, et al. Endoscopic Diagnosis and Management of Nonvariceal Upper Gastrointestinal Hemorrhage: European Society of Gastrointestinal Endoscopy Guideline-Update 2021. Endoscopy 2021; 53: 300-32.
- Barkun A, Alali A. What is the Current Role of an Over-the-Scope Clip Used as First-Line Endoscopic Hemostasis in Paitents with Nonvariceal Upper Gastrointestinal Bleeding. Ann Intern Med 2023; 176: 576-77.
- Meier B, Wannhoff A, Denszer U, et al. Over-the-Scope Clips versus Standard Treatment in High-Risk Patients with Acute Non-variceal Upper Gastrointestinal Bleeding: A randomised controlled trial (STING-2) Gut 2022; 71: 1251-58.
- Lee JH, Kedia P, Stavropoulos S, Carr-Locke D. AGA Clinical Practice Update on Endoscopic Management of Perforations in Gastrointestinal Tract: Expert Review. Clin Gastroenterol Hepatol 2021; 19: 2252-61.e2.

