Early Colonoscopy for Acute Lower GI Bleeding Usually Is Not the Answer
Shria Kumar, MD, MSCE
Assistant Professor, Division of Digestive and Liver Diseases, University of Miami Miller School of Medicine, Miami, Florida
This article reviews Shiratori, Y, Ishii N, Aoki T, et al. Timing of colonoscopy in acute lower GI bleeding: a multi-center retrospective cohort study. Gastrointest Endosc 2023 Jan;97(1):89-99.e10.
Access the article through PubMed
Correspondence to Shria Kumar, MD, MSCE. Associate Editor. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Is early colonoscopy (<24 hours) beneficial to reduce rebleeding or other clinically important outcomes compared to colonoscopy performed electively (24-48 hours) or late (48-120 hours) for patients hospitalized with an acute lower gastrointestinal bleed (LGIB)?
Design: Multicenter, retrospective study of patients who underwent a colonoscopy within 120 hours of admission for a LGIB.
Setting: Forty-nine hospitals in Japan.
Patients: Patients were from the CODE-BLUE-J study1 of people hospitalized with acute LGIB at 49 participating hospitals in Japan. Exclusion criteria included: patients who had prior LGIB; patients who did not receive a colonoscopy (or received it after 120 hours); patients who had post-procedural bleeding, colorectal cancer, or other neoplasms; patients with an upper GI bleed; or those who had bleeding after a colorectal surgery. A total of 6,270 patients were identified.
Exposures: Patients were identified to have undergone early (within 24 hours), elective (24-48 hours), or late (48-120 hours) colonoscopy.
Outcomes: Primary outcome was 30-day rebleeding rate, defined as a significant quantity of fresh blood loss or passage of wine-colored stools after colonoscopy, associated with any of the following: systolic blood pressure <100 mm Hg, pulse rate ≥ 100 beats/min, or >2 g/dL decrease in hemoglobin. Secondary outcomes included: (a) stigmata of recent hemorrhage, defined as the presence of active bleeding, detection of vessel or adherent clot; (b) 30-day mortality; (c) need for interventional radiology or surgery during the admission and after colonoscopy; (d) blood transfusion; and, (e) length of hospital stay, measured in days.
Statistical Analysis: This was a retrospective study that used inverse probability of treatment weighting to adjust for baseline characteristics. They then created propensity scores to account for covariates that would predict timing of colonoscopy, and performed inverse probability of treatment weighting to adjust for baseline characteristics among groups. The purpose of these steps is to mimic a randomized control trial in a retrospective study – where the baseline covariates are balanced between the arms of the study (in this case, early, elective, or late colonoscopy).
Results: Patients were identified to have undergone early (n=4,133), elective (n=1,137), or late (n=1,000) colonoscopy. Compared to both the elective and late groups, the early group had increased rate of identification of stigmata of recent hemorrhage, more endoscopic therapies performed, and a shorter length of hospital stay. However, the early group also had a higher 30-day rebleeding rate. There were no significant differences in the requirement for interventional radiology or surgery procedures, mortality, and transfused packed red blood cells among the groups. The findings are summarized in Table 1.
A subgroup analysis based on shock index (which reflects hemodynamic stability) and performance status (which reflects level of functioning, higher performance status is worse) found a benefit in early colonoscopy. Early colonoscopy had a significantly lower intervention or surgery requirement in the shock index ≥1 cohort (odds ratio [OR] 0.27; 95% confidence interval [CI], 0.10-0.72) compared with late colonoscopy. There was an interaction with performance status, with markedly divergent odds of rebleeding among those with poor performance status (≥3), in early vs late (ref) colonoscopy: performance status 0-2: OR 2.48, 95% CI, 1.90-3.24 and performance status ≥3: OR 0.46, 95% CI, 0.16-1.28.
Funding: Research support was provided by the Ministry of Health, Labor and Welfare, Japan, JSPS KAKENHI, Smoking Research Foundation, Takeda Science Foundation, and Grants-in-Aid for Research from the National Center for Global Health and Medicine.
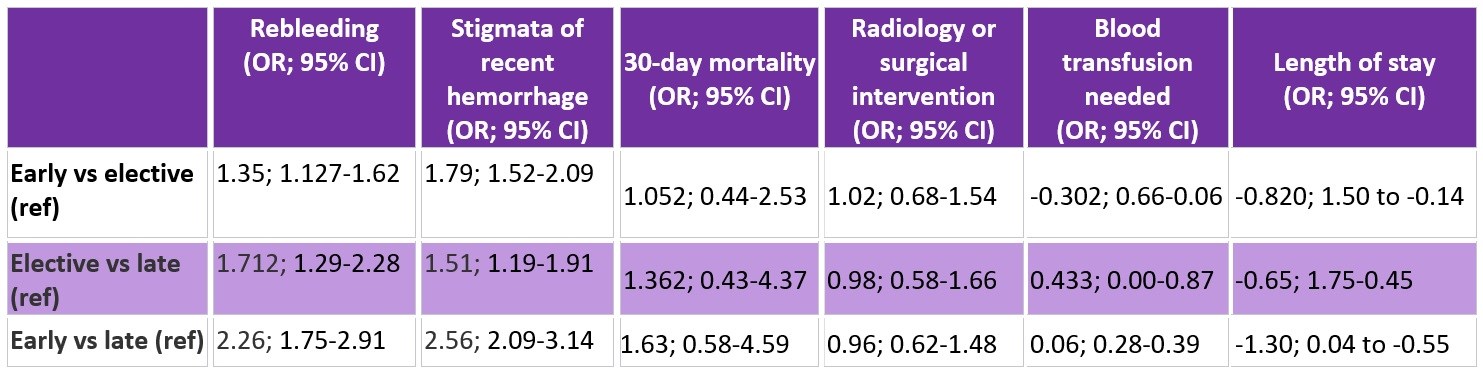
Table 1: Odds ratios of outcomes between colonoscopy timing. CI, confidence interval; OR, odds ratio.
COMMENTARY
Why Is This Important?
Acute LGIBs pose a dilemma – as gastroenterologists, we know that colonoscopy plays an important role in diagnosis of the LGIB etiology, but that endoscopic therapy is limited. Previously, the 2016 ACG guideline2 recommended a rapid bowel purge following hemodynamic resuscitation with colonoscopy performed within 24 hours to improve diagnostic and therapeutic yield. This contrasted with the British Society of Gastroenterology and the European Society of Gastrointestinal Endoscopy guidelines, which do not recommend early colonoscopy.3,4 This lack of consensus was driven by conflicting literature prior to 2016.5 While systematic reviews and meta-analyses have found at least higher rates of stigmata of recent hemorrhage and endoscopic intervention when colonoscopy is performed within 24 hours,6-8 2 recent small randomized controlled trials (RCTs) have found no improvement in rebleeding or mortality with early colonoscopy.9-10
These data led to an updated 2023 American College of Gastroenterology (ACG) guideline: “we recommend per-forming a nonemergent inpatient colonoscopy, as performing an urgent colonoscopy within 24 hours has not been shown to improve clinical out-comes.”11 Nevertheless, confirmatory data is needed. The authors of the present study note the difficulty in performing RCTs for acute LGIBs–particularly as it relates to sample size and ensuring populations are representative of what is seen in the real world, but also the limitations in observational studies, which can lack granularity. This well-designed study attempts to correct for the shortcomings of both by mimicking a RCT with observational data, and its findings provide further support for the new ACG guideline recommendation.
Key Study Findings
Subgroup analyses showed that those with moderate or severe shock or those with poor performance status may benefit from early colonoscopy. Specifically, early colonoscopy in the moderate-severe shock group led to fewer additional procedures by radiology or surgery, and there was a non-significant decrease in rebleeding rate for the poor performance status group.
Caution
Given the retrospective nature of this study, there are some methodologic limitations that could not be overcome. The authors use propensity scores and inverse probability of treatment weighting to overcome the lack of randomization in study design. Although this could still lead to bias and can be susceptible to unmeasured confounders, the authors do an excellent job of showing the findings for the observed, imputed, and weighted imputed data. Also, they excluded anyone who did not receive a colonoscopy, which may reflect an exclusion bias itself. Lastly, it’s hard to understand why the early group had a higher rebleeding rate, and particularly why those with poor performance status may benefit from early colonoscopy.
My Practice:
The updated ACG guidelines reflect my practice well. I generally recommend colonoscopy for hospitalized patients–but like the new guidelines, I consider whether the bleeding has stopped based on the patient’s hemodynamic status and response to resuscitation. Among those persons who have undergone a computed tomography (CT) angiogram in the emergency room with evident extravasation, I recommend interventional radiology evaluation and embolization urgently. Otherwise, I recommend resuscitation, ideally holding anticoagulants, and a nonurgent inpatient colonoscopy. This study really bolsters that approach for me, but also highlights a new area of interest, that those with moderate-severe shock or poor performance status may be served by early colonoscopy. Personally, these subgroups may be similarly or better served by early CT angiogram and I am more apt to send them for CT angiogram (if their creatinine allows) than urgently perform a colonoscopy with attempts at rapid bowel purge.
For Future Research
I would like to see further evaluation of the authors’ finding that those with poor performance status or high shock index can benefit in terms of early colonoscopy. In particular, I would want to know if CT angiogram provides the same (or greater) benefit in these groups, and if it is a more cost-effective approach. That the early group also had higher rebleeding rates similarly suggests that CT angiogram may be an appropriate first step for durable hemostasis. Parsing these out could identify which subgroups of patients warrant early colonoscopy, which is especially critical given the resource intensive nature of colonoscopy.
Conflict of Interest
Dr. Kumar reports no potential conflicts of interest.
REFERENCES
- Nagata N, Kobayashi K, Yamauchi A, et al. Identifying bleeding etiologies by endoscopy affected outcomes in 10,342 cases with hematochezia: CODE BLUE-J Study. Am J Gastroenterol 2021; 116: 2222-34.
- Strate LL, Gralnek IM. ACG Clinical Guideline: Management of Patients With Acute Lower Gastrointestinal Bleeding. Am J Gastroenterol Apr 2016;111(4):459-74.
- Oakland K, Chadwick G, East JE, et al. Diagnosis and management of acute lower gastrointestinal bleeding: guidelines from the British Society of Gastroenterology. Gut May 2019;68(5):776-789.
- Triantafyllou K, Gkolfakis P, Gralnek IM, et al. Diagnosis and management of acute lower gastrointestinal bleeding: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy Aug 2021;53(8):850-868.
- Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol Dec 2010;105(12):2636-41; quiz 2642.
- Sengupta N, Tapper EB, Feuerstein JD. Early Versus Delayed Colonoscopy in
Hospitalized Patients With Lower Gastrointestinal Bleeding: A Meta-Analysis. J Clin Gastroenterol Apr 2017;51(4):352-359. - Kherad O, Restellini S, Almadi M, et al. Systematic review with meta-analysis: li-mited benefits from early colonoscopy in acute lower gastrointestinal bleeding. Aliment Pharmacol Ther Sep 2020;52(5):774-788.
- Tsay C, Shung D, Stemmer Frumento K, Laine L. Early Colonoscopy Does Not Improve Outcomes of Patients With Lower Gastrointestinal Bleeding: Systematic Review of Randomized Trials. Clin Gastroenterol Hepatol Jul 2020;18(8):1696-1703 e2.
- van Rongen I, Thomassen BJW, Perk LE. Early Versus Standard Colonoscopy: A Randomized Controlled Trial in Patients With Acute Lower Gastrointestinal Bleeding: Results of the BLEED Study. J Clin Gastroenterol Sep 2019;53(8):591-598.
- Niikura R, Nagata N, Yamada A, et al. Efficacy and Safety of Early vs Elective Colonoscopy for Acute Lower Gastrointestinal Bleeding. Gastroenterology Jan 2020;158(1):168-175 e6.
- Sengupta N, Feuerstein J, Jairath V, et al. Management of Patients with Acute Lower Gastrointestinal Bleeding: An Updated ACG Guideline. Am J Gastroenterol 2023; 118: 208-31.
Download the Article Summary (PDF)


