Free Online Program Improves Adenoma Detection Rate and Decreases Post-Colonoscopy Colorectal Cancer
 Jeffrey Lee, MD, MPH
Jeffrey Lee, MD, MPH
Research Scientist and Attending Gastroenterologist, Kaiser Permanente San Francisco Medical Center, San Francisco, CA
This article reviews Corley DA, Jensen CD, Lee JK, et al. Impact of a Scalable Training Program on the Quality of Colonoscopy Performance and Risk of Post-Colonoscopy Colorectal Cancer. [Published ahead of print April 22, 2023]. Gastrointest Endosc. doi: 10.1016/j.gie.2023.04.2073
Access the article through PubMed
Correspondence to Jeffrey Lee, MD, MPH. Associate Editor. Email: EBGI@gi.org
STRUCTURED ABSTRACT
Question: Is a 30-minute, interactive, online educational program about quality of colonoscopy associated with an increased adenoma detection rate (ADR) and decreased risk of post-colonoscopy colorectal cancer (CRC)?
Design: Retrospective cohort study with endoscopists serving as their own controls, pre- and post-online education.
Setting: Kaiser Permanente Northern California endoscopy centers (n =21).
Study Population: All gastroenterologists practicing at Kaiser Permanente Northern California sites in 2014, who completed > 100 colonoscopies/year with >25 screening exams/year during the 3-year period before and after online training (n = 86).
Intervention/Exposure: Completion of 30-minute, interactive, online training about quality of colonoscopy during a 3-month training period in 2014. Using behavior-change theory, research on evidence-based interventions, and identified drivers of ADR variability, the training program reviewed optimal colonoscopy exam techniques, identification of flat adenomas, and social incentives for normalizing a quality-focused culture. The online training program is available for free at https://deliveryscience-appliedresearch.kaiserpermanente.org/specialty-research-networks/gastroenterology-hepatology.
Outcome: The primary outcome was change in individual endoscopist’s ADR derived from average-risk screening colonoscopies during the 3-year post-training period compared to 3-year pre-training period. The secondary outcome was association between endoscopists’ ADR and their patients’ risk of post-colonoscopy CRC.
Data analysis: Interrupted time series analysis, adjusted for temporal trends in ADR. Cox proportional hazards regression used to assess association between ADR and risk of post-colonoscopy CRC to produce adjusted hazards ratio (aHR).
Funding: National Cancer Institute.
Results: Among 86 study endoscopists, 133,225 colonoscopies were performed in the pre-training period with 23.8% performed for CRC screening (n=31,643), and 146,786 colonoscopies performed during the post-training period with 19.4% performed for CRC screening (n=28,408). Patient characteristics were similar in pre- and post-training period: median age = 63; 51% female; 61-63% White; and body mass index (BMI)=27.3.
Median ADR rose from 29.2% (interquartile range [IQR]: 22.8%-35.1%) in the pre-training period to 35.5% (IQR: 31.3%-44.5%) in the post-training period. In the initial 3-month period following training, mean ADR increased by 3.13%. This increase was greatest for endoscopists whose pre-training ADR was below the group’s median ADR of 29.2% (Figure 1). Each 1% increase in ADR was associated with a 4% decrease in their patients’ risk of post-colonoscopy CRC (aHR = 0.96; 95% confidence interval: 0.93-0.99).
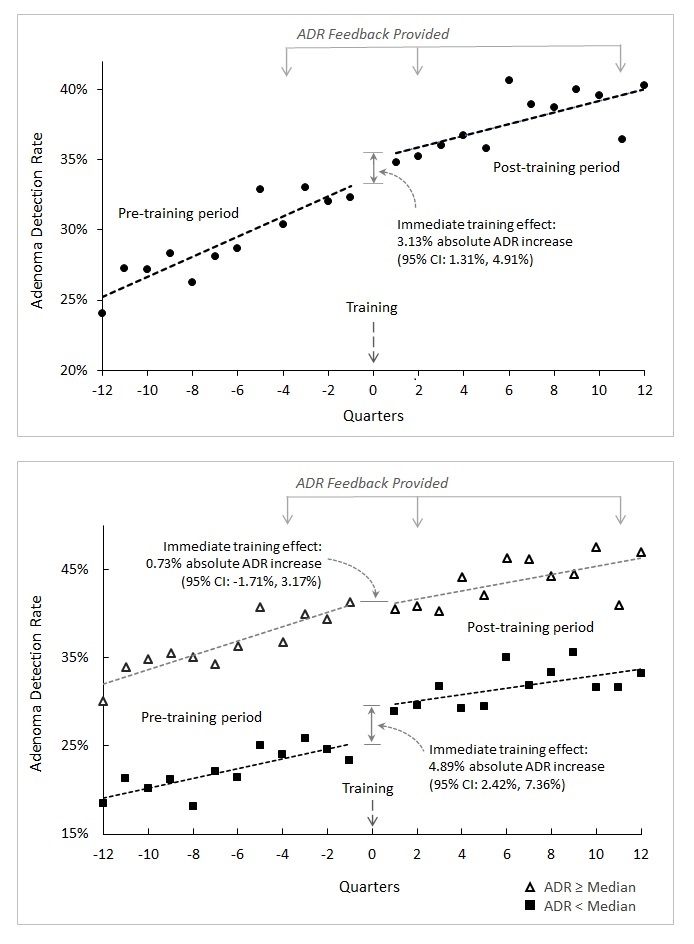
Figure 1. Endoscopist adenoma detection rate pre– and post-training.
ADR, adenoma detection rate; CI, confidence interval.
COMMENTARY
Why Is This Important?
The beneficial effect of colonoscopy on reducing CRC incidence and mortality is largely derived from early detection and removal of adenomas.1 Studies have consistently shown the magnitude of this benefit varies based on the quality of the colonoscopy examination, particularly the ability to detect adenomas.2,3 To improve colonoscopy quality, multiple guidelines recommend physician ADR benchmarks of ≥25%.4 Despite its widespread adoption as a key colonoscopy quality measure in clinical practice, there are still significant variation in ADR among endoscopists.2,3 As such, numerous interventions have been developed to enhance ADR including increased emphasis on withdrawal times to 9 minutes, recommending a second look or retroflexing in the right colon, and use of distal attachment and artificial intelligence devices.5 While many of these interventions have shown to improve ADR, they can be costly, difficult to implement, or require additional in-person training. Thus, this study addresses an important gap in implementation by developing a 30-minute online training program aimed to improve ADR while being freely available for all endoscopists. Importantly, this easily scalable intervention was shown to improve ADR among endoscopists from the study while also reducing the risk of post-colonoscopy CRC.
A freely available 30-minute online training program was associated with a mean absolute increase in physician ADR of 3.1%. The effect was more pronounced among endoscopists who had ADRs below the median pre-training ADR of 29.2% compared to those above the median. (i.e., 4.9% increase versus 0.7% increase, respectively). Post-training, each 1% absolute increase in ADR among endoscopists was associated with a 4% decrease in their patients’ PCCRC risk.
Caution
The main limitation of this study is that it was not a randomized controlled trial; however, the study used a pre- and post-training design that allowed endoscopists to serve as their own control and the interrupted time series analysis controlled for temporal trends in ADRs. Another limitation is that this study took place in a setting where ADR feedback was provided annually.
My Practice
In our large medical group consisting of over 160 gastroenterologists across 21 medical centers, screening and overall ADRs along with other quality metrics (e.g., cecal intubation rate, etc.) are provided annually to all gastroenterologists to facilitate self-assessment and performance improvement. In addition to measuring ADR, our organization has provided the 30-minute online training program to all gastroenterologists and has required it for all new hires.
In my personal practice, I use several tools and techniques that are highlighted in this online training program to optimize adenoma detection. First, it is critical to use a high-definition colonoscope with image enhancement (e.g., narrow band imaging) capabilities to help detect and evaluate subtle lesions. Second, it is important to understand all the subtle features of flat polyps and have mindset for detecting flat polyps since these lesions are often missed. Third, I maximize mucosal exposure by working the folds (i.e., deflecting the tip of the colonoscope into the inner-haustral valley and exposing the proximal sides of each haustral folds), cleaning and suctioning any stool debris, and distending the lumen adequately. Fourth, I perform 2 or 3 passes in the right colon since adenomas are often missed in this location. Lastly, when available, I often use a distal attachment device such as a clear translucent cap to help expose the proximal sides of each haustral fold and improve mucosal exposure.
For Future Research
A randomized trial evaluating this online training program in a different setting would improve the generalizability of this study’s findings. In addition, testing whether this freely available online training program can improve proximal serrated detection rates, which has been shown to be variable among endoscopists and is associated with PCCRC, should be performed.
Conflict of Interest
Dr. Lee was a co-author and investigator of this study.
@douglascorley
@jessicachubak
@jeffleemd
REFERENCES
- US Preventive Services Task Force. Screening for colorectal cancer: US Preventive Services Task Force recommendation Statement. JAMA 2016;315(23):2564-2575.
- Corley DA, Jensen CD, Marks AR, et al. Adenoma detection rate and risk of colorectal cancer and death. N Engl J Med 2014;370(14):1298-1306.
- Kaminski MF, Regula J, Kraszewska E, et al. Quality indicators for colonoscopy and the risk of interval cancer. N Engl J Med. 2010;362(19):1795-1803.
- Rex DK, Schoenfeld PS, Cohen J, et al. Quality indicators for colonoscopy. Gastrointest Endosc. 2015;81(1):31-53.
- Shaukat A, Tuskey A, Rao VL, et al. Interventions to improve adenoma detection rates for colonoscopy. Gastrointest Endosc 2022 ;96(2):171-183.

