ESD vs EMR for Large Nonpedunculated Colon Polyps: Fewer Recurrences but More Complications
 Jeffrey Lee, MD, MPH
Jeffrey Lee, MD, MPH
Research Scientist and Attending Gastroenterologist, Kaiser Permanente San Francisco Medical Center, San Francisco, CA
This summary reviews Jacques J, Schaefer M, Wallenhorst T, et al. Endoscopic en bloc versus piecemeal resection of large nonpedunculated colonic adenomas: A randomized comparative trial. Ann Intern Med 2024; 177: 29-38.
Access the article through PubMed
Correspondence to Jeffrey Lee, MD, MPH. Associate Editor. Email: EBGI@gi.org
Keywords: colonoscopy, polypectomy, endoscopic submucosal dissection, adenomas
STRUCTURED ABSTRACT
Question: Does endoscopic submucosal dissection (ESD) decrease incomplete polyp resection/polyp recurrence of large (≥25 mm) colon polyps with similar rates of adverse events compared to conventional piecemeal endoscopic mucosal resection (EMR)?
Design: Multi-center, prospective, randomized, comparative trial (RESECT-COLON trial).
Setting: Six French referral centers from November 2019 through February 2021, with colonoscopies performed by 13 experienced endoscopists.
Patients: Adults >18 years old referred for endoscopic resection of large (≥25 mm) colon polyps consistent with laterally spreading tumors (LST) that were ≥15 mm from anal verge (i.e., excluded rectal lesions) and with no endoscopic features of deep submucosal invasion. LST and Paris classification used to categorize polyp characteristics.
Interventions: Patients were randomly assigned (1:1 ratio) to EMR or ESD with stratification for center and polyp location. For all colonoscopies, patients had general anesthesia with intubation, had the procedure performed as an inpatient and were hospitalized for 1 night after the procedure, which is the French standard. Submucosal fluid injection was performed prior to all polypectomies. The choice of endoscope, injection fluid and specific ESD/EMR devices were at the discretion of the endoscopist. ESD included dissection around and underneath the lesion to achieve en bloc resection while EMR was performed with piecemeal polypectomies with snare-tip thermal ablation at polypectomy margins. Clip closure of resection site was performed at the discretion of the endoscopist.
Outcomes: Primary outcome was neoplastic recurrence at polypectomy site found during 6-month follow-up colonoscopy. All polypectomy scars were biopsied. Secondary endpoints included frequency of adverse events and procedure time among others.
Data Analysis: Intention-to-Treat and per-protocol analyses were reported. Sample size was calculated assuming 10% recurrence rate in EMR and 2% recurrence with ESD.
Funding: French Ministry of Health.
Results: Among 360 randomized patients, mean age was 69-71 years old, 39%-47% were female, right colon location in 77%, and 85% were Paris Classification 0-IIa. Failure to compete procedure rates were low for ESD and EMR (3.4% and 1.6%, respectively), and en bloc resection rate was significantly higher with ESD vs EMR (96.6% vs 10.4%, respectively). Recurrence rate was significantly lower with ESD (1/161, or 0.6%) vs EMR (8/157, or 5.1%) (Figure 1). ESD required significantly more time to complete compared to EMR: 47 minutes vs 14.5 minutes, respectively. Among patients treated with EMR with recurrent neoplasia at 6 months, complete endoscopic resection of residual neoplasia was achieved in all patients.
Adverse events were significantly higher with ESD vs EMR: 35.6% vs 24.5%, respectively; relative risk (RR) 1.40; 95% confidence interval (CI): 1.0-2.0. Specifically, frequency of post-polypectomy syndrome was significantly higher with ESD (11.8% vs 5.5%, respectively; RR 2.2; 95% CI: 1.1-4.5) and were numerically higher with ESD for periprocedural perforation (5.6% vs 2.2%), clinically significant post-procedural bleeding (7.9% vs 5.5%), and surgery for complications (1.1% vs 0%).
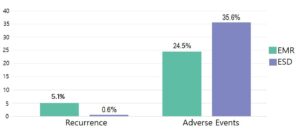 Figure 1. Recurrence rates and adverse events. P <0.05 for both comparisons.
Figure 1. Recurrence rates and adverse events. P <0.05 for both comparisons.EMR, endoscopic mucosal resection; ESD, endoscopic submucosal dissection.
COMMENTARY
Why Is This Important?
Endoscopic resection is the preferred approach for the management of large non-pedunculated colorectal polyps ≥20 mm. Current guidelines recommend expert endoscopic assessment of all large, non-pedunculated colorectal polyps before surgical consideration.1,2 In the United States and other Western countries, EMR, frequently performed with submucosal injection, has been the preferred endoscopic technique for the management of large, non-pedunculated colorectal polyps ≥20 mm due to its efficiency, low recurrence rates (5%-20%), and favorable safety profile,1,3 although en bloc resection of large polyps may not be feasible for all large polyps, leading to the performance of multiple smaller or piecemeal resections with recurrence of neoplasia minimized by using snare-tip soft coagulation of polypectomy margins.
ESD is a newer endoscopic technique that was developed in the East and is now gaining wider adoption in the West. The advantage of ESD is that it provides the ability to remove all large, non-pedunculated colorectal polyps en bloc, which allows for complete staging and the potential cure of superficial submucosal invasive cancer (i.e., malignant invasion limited to the upper third of the submucosa). In order to do this, ESD usually includes submucosal injection, followed by pre-cutting the mucosa surrounding the polyp, and then dissecting the connective tissue of the submucosa beneath the polyp using specialized cutting tools. In addition to facilitating en bloc resection, ESD produces lower recurrence rate (<2%). However, ESD is technically complex. It may be taught during an advanced endoscopy fellowship or could be learned with observation, proctoring with a skilled endoscopist, and training on animal models prior to independent performance. ESD also has a higher adverse event rate (e.g., perforation)1 and requires substantially more time to perform compared to EMR.
Given these differences between EMR and ESD, it remains unclear which endoscopic technique is preferable for the management of large, non-pedunculated colorectal polyps, and the authors should be congratulated for conducting a well-designed randomized controlled trial (RCT) to address this important issue. This is the definitive RCT to compare the safety and effectiveness of EMR and ESD for large colonic adenomas
Key Study Findings
Also, ESD required significantly more time than ESD than EMR (47 minutes vs 14.5 minutes).
Caution
This study was conducted among experts in ESD and EMR who have years of experience and their recurrence rates and adverse event rates may not be generalizable in other settings. In addition, the study included sessile serrated lesions, which may not be the ideal lesion for ESD given its low risk of harboring any low-risk submucosal invasive cancer (SMIC) and ease of resection with more safer and effective methods (e.g., piecemeal cold EMR). Also, patients with rectal lesions were excluded. Although the rationale for this was not detailed in the publication, it’s probably because ESD is considered the optimal technique for large rectal adenomas, especially if there is evidence of low-risk, superficial submucosal invasive cancer.4
My Practice
When I encounter a large (i.e., ≥20 mm) or complex polyp during a screening or diagnostic examination, the first question I ask is whether it has any deep submucosal invasive features by examining the lesion on high-definition white light (HDWL) and image enhanced endoscopy (e.g., narrow band imaging (NBI), bioluminescence imaging, i-scan, etc.) and using my polyp classification schemes (Paris classification, NBI International Colorectal Endoscopic [NICE], and Japan NBI Expert Team). If there’s overt signs of deep submucosal invasive disease (e.g., NICE Type III, Paris III, excavation or ulceration), I would biopsy the lesion to confirm and refer this lesion to surgery. If there’s uncertainty regarding any features of deep submucosal invasive, it is reasonable to call a colleague for a second opinion or refer the lesion to an expert advanced resection center. If there is no evidence of any deep submucosal invasive features on HDWL or NBI, then the next question is whether there are any high-risk features of superficial submucosal invasive (e.g., increasing laterally spreading tumor (LST) size, rectal location, LST non-granular appearance, Paris IIc morphology, etc.). If so, these lesions should be resected en bloc using either ESD or EMR, depending on the size. If there’s no high-risk features or evidence of superficial or deep submucosal invasion, EMR (either en bloc or piecemeal) is an efficient, safe, and effective approach to remove large, non-pedunculated colorectal polyps.
Although I did not complete an advanced endoscopy fellowship, I learned ESD techniques after appropriate observation, proctoring with hands-on training, and practice on animal models. I limit my practice to performing ESD on large rectal lesions, especially if there is evidence of superficial submucosal invasion since it’s important to achieve en bloc resection in these patients. Given the thickness of the rectal wall, the risk of perforation is lower and performance of ESD allows the patient to forego rectal surgery, which is more likely to lead to colostomy and usually has a greater impact on quality of life compared to segmental resection in other sections of the colon.
For Future Research
Additional studies are needed to determine the most safe and effective endoscopic resection method for large, non-pedunculated polyps in the rectum.
Conflict of Interest
Dr. Lee reports no conflicts of interest.
REFERENCES
- Kaltenbach T, Anderson JC, Burke CA, et al. Endoscopic removal of colorectal lesions— recommendations by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc 2020;91:486-519.
- Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMR): European Society of Gastrointestinal Endoscopy (ESGE) clinical guideline. Endoscopy 2017;49:270-297.
- Sidhu M, Shahidi N, Gupta S, et al. Outcomes of thermal ablation of the mucosal defect margin after endoscopic mucosal resection: a prospective, international, multicenter trial of 1000 large nonpedunculated colorectal polyps. Gastroenterology 2021;161:163-170.e3.
- Burgess NG, Bourke MJ. Endoscopic submucosal dissection versus endoscopic mucosal resection of large colon polyps: use both for the best outcomes. Annal Intern Med 2024; 177: 89-90.

