When to Discontinue CRC Screening in Older Adults: Chronological Age or Life Expectancy?

Philip N. Okafor, MD, MPH
Senior Associate Consultant, Department of Gastroenterology, Mayo Clinic, Jacksonville, Florida
This summary reviews Liu PH, Singal AG, Murphy CC. Colorectal cancer screening receipt does not differ by 10-year mortality risk among older adults. Am J Gastroenterol 2024;119: 353-363.
Access the article through PubMed
Correspondence to Philip N. Okafor, MD, MPH, Associate Editor. Email: EBGI@gi.org
Keywords: colon cancer, screening, geriatrics, colonoscopy, life expectancy
Question: Among older adults (65-84 years) in the US, how often is colorectal cancer (CRC) screening performed in relation to 10-year mortality risk?Design: Retrospective cross-sectional study using data from the National Health Interview Survey (NHIS) conducted by the National Center for Health Statistics.
Setting: Community-dwelling adults in the US.
Participants: Adult respondents of the National Health Interview Survey aged 65 to 84 years who were not up to date on CRC screening. Individuals residing in long-term care facilities, living abroad, or incarcerated were excluded from the study. Participants with missing information on CRC screening and those who were up to date with CRC screening were also excluded.
Intervention/Exposure: Completion of CRC screening (colonoscopy, sigmoidoscopy, or stool-based tests).
Outcomes: The primary outcome was the prevalence of CRC screening in the preceding 12 months, regardless of indication, among individuals who were not up to date with CRC screening, stratified by 10-year mortality risk. Other outcomes included the proportion of CRC screening performed among adults with a life expectancy <10 years (i.e., 10-year mortality risk ≥50%) and the association between quintile of mortality index and receipt of past year screening. This was reported as odds ratios (OR) and confidence intervals (CI).
Data Analysis: Ten-year mortality risk was estimated using the Schonberg mortality index developed via NHIS data linked with the National Death Index. This was then used to estimate 10-year life expectancy. The prevalence of past-year CRC screening was assessed by quintiles of mortality risk (quintile 1 = lowest risk, quintile 5 = highest risk) and age group. The association between mortality risk and past-year screening was evaluated using logistic regression after controlling for potential confounders. Other exploratory analyses included the prevalence of past-year screening by combinations of 5-year age group, mortality risk quintile, type of CRC screening modality, and the proportion of screening performed in adults with less than 10 years of life expectancy.
Funding: National Institutes of Health
Results: Among the entire cohort of 25,888 adults, the proportion of individuals who were not up to date with CRC screening was highest in the 65–69-year age group (35.8%) and lowest in the 80-84-year age group (13.3%). The prevalence of past-year screening in the entire cohort was 38.5%. According to mortality risk quintiles, the prevalence of past-year screening ranged from 39.5% in the lowest quintile to 35.4% in the highest quintile (Figure 1). Receipt of CRC in the past year was not associated with the mortality index quintile (OR 1.05, 95% CI 0.93-1.2). Interestingly, within some 5-year age groups, such as the 65–69-year age group, the prevalence of past-year screening was similar by quintile of mortality risk. However, within other groups like the 75–79-year age group, the prevalence of past-year screening increased with increasing or higher mortality risk (P=0.02). About 28% of past-year screening was performed in adults with a life expectancy <10 years. This increased from 13.7% in the 65–69-year age group, to 65.6% in the 80–84 year age group (Table 1).
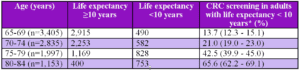
*Weighted percentage and 95% confidence intervals
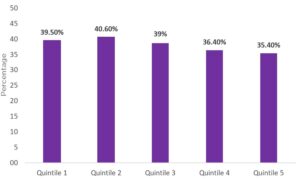 Figure 1. Prevalence of colorectal cancer screening by 10-year mortality risk quintile.
Figure 1. Prevalence of colorectal cancer screening by 10-year mortality risk quintile.Quintile 1= lowest 10-year mortality risk; Quintile 5= highest 10-year mortality risk
COMMENTARY
Why Is This Important?
Older Americans are estimated to make up 21% of the entire population by 2030.1 By 2060, nearly 1 in 4 Americans will be 65 years or older.1 As such, more adults than ever will be faced with deciding when to stop CRC screening. At present, the latest United States Preventative Services Task Force recommendations suggest clinicians selectively offer CRC screening in adults 76 to 85 years old because evidence indicates that the net benefit is small.2 They also recommend consideration of overall health, prior screening history, and patient preferences.2 As a result, many providers use the chronological age of 75 years as the major consideration in discontinuing CRC screening. However, recent studies have suggested that we may be over screening patients for CRC.3,4 Conversely, we may also be underscreening some patients over 75 years with longer life expectancy.
In this study, Liu et al make the case for a shift in the way the decision to stop CRC screening is approached, suggesting we move away from using only the chronological age. Instead, they recommend that life expectancy and overall health status should play a more important role in the decision to stop CRC screening. They show that CRC screening is being performed among patients with a life expectancy of fewer than 10 years, comparable with the findings of Calderwood et al who also showed significant rates of CRC screening among patients with a life expectancy of less than 5 years in New Hampshire.3 The results of Liu et al become more compelling when you consider recent evidence that the rates of invasive CRC among patients screened over the age of 75 years is very low and that these patients are more likely to have complications than younger patients.4 Also, even among older adults diagnosed with CRC, only a small proportion will choose to receive treatment for malignancy.4
Key Study Findings
The study suggests that life expectancy and overall health status are not always considered by healthcare providers when recommending CRC screening in adult patients.
Caution
While the NHIS is a nationally representative sample, participant responses are self-reported and as such, not validated by the investigators. In addition, given the nature of the NHIS, the authors were also unable to reliably ascertain if the CRC screening modality was truly done for screening purposes vs surveillance or diagnostic indications. The authors also allude to the fact that the reported mortality index used for the study shows good discrimination at the population level but may not be as precise at the individual level.
My Practice
In the US, most recommendations for CRC screening come from primary care. As such, most screening colonoscopies I perform are from open-access referrals. When I do see an elderly patient in the clinic who requests a screening colonoscopy, I try to carry out shared decision-making, emphasizing the risks vs benefits of invasive CRC screening and the prevalence of CRC in previously screened individuals of a similar age profile. I also discuss their thoughts on treatment if a malignancy was found during CRC screening. I often find these conversations challenging because of the sensitive nature of life expectancy and mortality risk. While online resources to estimate mortality risk exist, they are not routinely used in clinical practice, and many providers are not trained on how to incorporate life expectancy discussions into the decision-making process for continued CRC screening. Importantly, I do find that when I emphasize that CRC screening or surveillance is no longer beneficial in the endoscopy report, it goes a long way in reassuring patients and primary care providers.
For Future Research
More efforts are needed to train providers on the incorporation of online tools for estimating mortality risk in the CRC screening decision-making process. Health systems should encourage quality improvement projects that can incorporate these tools into real-time cancer screening calculators. The impact of these tools on the prevalence of CRC screening among the elderly needs to be studied. Providers need to be trained on the proper way to have conversations regarding discontinuing CRC screening via shared decision-making. Audit and feedback for clinicians on their patients’ CRC screening rates in relation to life expectancy is deserving of further study. Finally, the perspectives of patients receiving these CRC screening recommendations that incorporate mortality risk and life expectancy need to be investigated qualitatively.
Conflict of Interest
Dr. Philip Okafor reported no potential conflicts of interest.
@docamitgs
Amit Singal
REFERENCES
- Vespa J. The Graying of America: More Older Adults Than Kids by 2035. https://www.census.gov/library/stories/2018/03/graying-america.html. Updated October 9, 2021. Accessed March 13, 2024.
- US Preventive Services Task Force. Colorectal Cancer: Screening. www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening. Published May 18, 2021. Accessed march 13, 2024.
- Calderwood AH, Tosteson TD, Wang Q, Onega T, Walter LC. Association of Life Expectancy With Surveillance Colonoscopy Findings and Follow-up Recommendations in Older Adults. JAMA Intern Med 2023;183(5):426-434.
- El Halabi J, Burke CA, Hariri E, et al. Frequency of Use and Outcomes of Colonoscopy in Individuals Older Than 75 Years. JAMA Intern Med 2023;183(6):513-519.

