It’s a Bad “Prep” Even Though the Patient Took It Correctly: Consider 15 mg Bisacodyl plus 4-Liter PEG Split Prep Before Next Colonoscopy

Philip Schoenfeld, MD, MSEd, MSc (Epi)
Chief (Emeritus)-Gastroenterology Section, John D. Dingell VA Medical Center, Detroit, MI
This article reviews Sey MSL, Von Renteln D, Sultanian R, et al. A Multicenter Randomized Controlled Trial Comparing Bowel Cleansing Regimens for Colonoscopy After Failed Bowel Preparation. Clin Gastroenterol Hepatol 2022; In Press.
Correspondence to Philip Schoenfeld, MD, MSEd, MSc (Epi), Editor-in-Chief. Email: EBGI@gi.org
repeat colonoscopy?
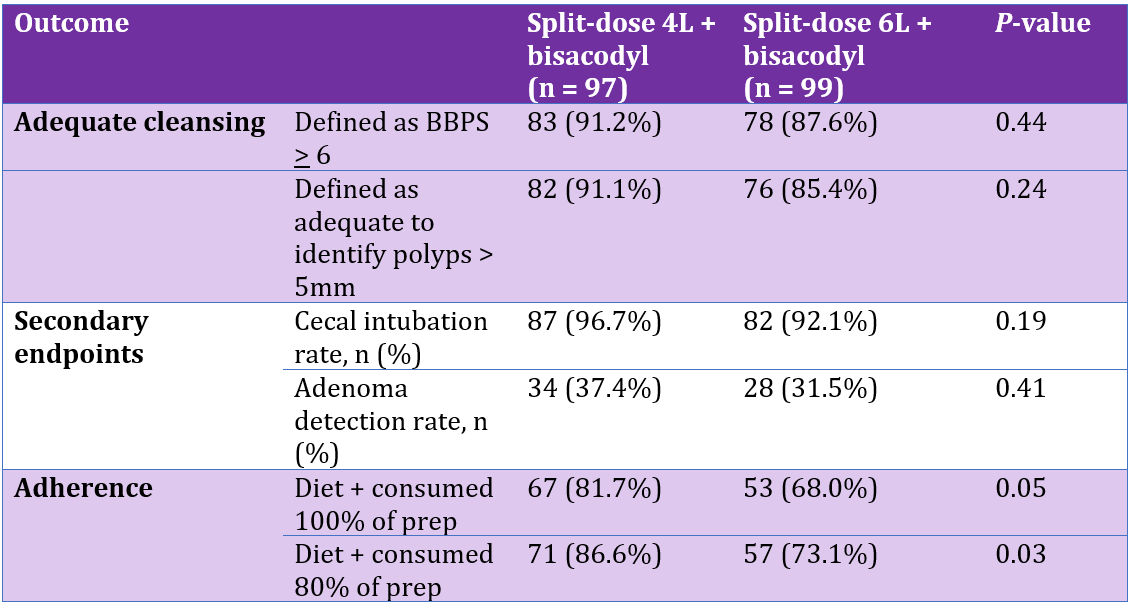
Table 1. Results
COMMENTARY
Why Is This Important?
It’s a frequent question for endoscopists: what prep should I use for patients who have inadequate cleansing despite being compliant with the initial prep? Even though endoscopists face this question daily, there is minimal data, especially for patients who initially used a 4L PEG split-prep. Gimeno-Garcia and colleagues did the only other RCT of 256 patients who had inadequate cleansing.1,2 Most (74.8%) had initially used a low volume bowel prep without reporting whether or not the prep was split. For the repeat colonoscopy, all study patients used 10 mg bisacodyl on the day before the procedure and followed a low-residue diet for 3 days pre-procedure. Patients were randomized to 4L PEG-3350 as split-prep vs 2L PEG + ascorbic acid as split-prep. The 4L PEG-3350 was superior for adequate bowel cleansing (81.1% vs 67.4%, P< 0.01, ITT analysis). Thus, 4L PEG-3350 split-prep may be helpful for compliant patients who failed a low-volume prep, although the adequate cleansing rate (81.1%) is still lower than the target of 85% of bowel preps with adequate cleansing.2
In the absence of other data, endoscopists may recommend a wide variety of inadequately studied regimens, including 2-days of clear liquids prior to colonoscopy and supplementing 4L PEG with magnesium citrate 1-2 days before colonoscopy. Finally, Sey, Barkun, and colleagues with the Canadian Bowel CLEANsing National Initiative have assessed supratherapeutic purgative regimens in a well-designed RCT, and should be congratulated for this effort.
Remember that there are multiple known risk factors for colonic dysmotility and inadequate bowel cleansing even when a patient is compliant, including obesity, current opioid use, diabetes mellitus, history of using constipation treatments, and current use of anticholinergics, including tri-cyclic antidepressants, among others.2 It appears that most patients in the current trial had one or more of these risk factors: 36.7% obese, 40.8% with history of constipation or IBS-C, approximately 10% using opioids, etc. However, if a patient is not compliant and has poor bowel cleansing (e.g., didn’t split the prep properly and drank it all on the previous evening), then additional patient education is likely to be more helpful than prescribing a supratherapeutic regimen.
Key Study Findings
Both supratherapeutic regimens were quite effective with no significant difference in rates of adequate bowel cleansing for 2 + 2L PEG + bisacodyl vs 4 + 2L PEG + bisacodyl regimens (91.2% vs 87.6%, P= 0.44). There was no evidence of effect modification in pre-planned secondary analyses based on presence of constipation/IBS-C, type of bowel preparation used initially, etc., although actual rates of adequate cleansing for these secondary analyses were not reported.
Caution
High doses of bisacodyl (20mg) as part of bowel regimens have been associated with a very small (0.48%) risk of colonic ischemia at the time of colonoscopy.3 Although this is usually an incidental finding, it contributed to the voluntary withdrawal of Half-Lytely, a combination of 2L PEG-3350 + 20, mg bisacodyl from the US market in 2010. Subsequently, even bowel preparation kits with 10mg bisacodyl were withdrawn from the US market.
The current trial is too small to identify an increased risk with 15mg bisacodyl. Nevertheless, given the need for a supratherapeutic bowel regimen in these study patients, I think that the risk-benefit ratio favors using this dose of bisacodyl in order to get good cleansing and a thorough exam of the colon. There were no differences in rates of adequate cleansing regardless of bowel regimen used at index colonoscopy. However, only a minority of patients used a 4L PEG split-prep initially, and it would be interesting to see the actual data for this difficult-to-treat group.
Our Practice
If a patient has been compliant with my standard prep (4L PEG-3350 split prep) and still has inadequate bowel cleansing, our group prescribes 6L PEG-3350 split-prep with 4L PEG consumed between 6 and 10 PM on the night before the procedure, and 2L consumed 4-6 hours before colonoscopy. This regimen produced adequate cleansing based on BBPS in 87.7% in an ITT analysis.4 Furthermore, we proactively prescribe this supratherapeutic regimen for any patient with 2 or more risk factors for inadequate bowel cleansing, and achieve adequate cleansing in 91.5% of these high-risk patients. Given the study findings from Sey, Barkun, and Canadian Bowel CLEANsing National Initiative, our group is planning to trial the 2 + 2L PEG + 15mg bisacodyl as our preferred supratherapeutic regimen and quantify rates of adequate cleansing as part of our ongoing quality improvement initiative. It’s worth re-emphasizing that more and better patient education is the preferred intervention when a patient is clearly non-compliant. For example, I don’t use a supratherapeutic regimen when a patient drinks all of their bowel prep on the evening before colonoscopy. My nursing team initially focuses on re-educating the patient on splitting the prep properly and scheduling the patient for a late-morning or early afternoon appointment if the patient is worried about rising early to take the second dose of bowel prep.
For Future Research
Future research should assess supratherapeutic regimens in a larger group of compliant patients who had inadequate cleansing after using 4L PEG-3350 in a split-prep. Also, a future RCT should compare a supratherapeutic regimen vs lower-volume bowel purgative regimen in patients with two or more risk factors for inadequate cleansing.
Conflict of Interest
Dr. Schoenfeld is a consultant, advisory board member and member of the Speaker’s Bureau for Salix Pharmaceuticals.
REFERENCES
1. Gimeno-Garcia AZ, Hernandez G, Aldea A, et al. Comparison of two intensive bowel cleansing regimens in patients with previous poor bowel preparation: a randomized controlled study. Am J Gastroenterol 2017; 112: 951-58.
2. Saltzman JR, Cash BD, Pasha SF, et al. Bowel Preparation before Colonoscopy. GIE 2015; 81: 781-94.
3. O’Reilly P, Burgart L, Vargo P. High Dose Bisacodyl as Part of a Colonoscopy Preparation May Cause Colon Ischemia. GIE 2009; 69: PAB 134. DOI: https://doi.org/10.1016/j.gie.2009.03.178.
4. Tama M, Kathi P, Schoenfeld P, et al. Bowel Preparation for Patients with History of Inadequate Cleansing with 4L PEG-3350 (GoLytely®) Split-Prep: The 6 Liter PEG-3350 (GoLytely®) Split-Prep. Am J Gastroenterol 2018; 114: A336.

