In Case You Missed It
Eating “Healthy” to Minimize Colon Cancer
 Philip Schoenfeld, MD, MSEd, MSc (Epi)
Philip Schoenfeld, MD, MSEd, MSc (Epi)
Chief (Emeritus), Gastroenterology Section, John D. Dingell VA Medical Center, Detroit, MI.
This summary reviews Wang L, Du M, Wang K, et al. Association of ultra-processed food consumption with colorectal cancer risk among men and women. BMJ 2022; 378:e068921.
Correspondence to Philip Schoenfeld, MD, MSEd, MSc. Editor-in-Chief. Email: EBGI@gi.org
Keywords: colorectal cancer, processed food, food frequency questionnaire, NOVA classification
STRUCTURED ABSTRACT
Question: Does high consumption of ultra-processed foods increase the risk of colorectal cancer (CRC)?
Design: Prospective cohort study of male clinicians from Health Professionals Follow-Up Study (1986-2014), and female nurses from Nurses’ Health Study I (1986-2014), and Nurses’ Health Study II (1991-2015).
Setting: The Health Professionals Follow-Up Study was established in 1986 with 51,529 male clinicians (physicians, optometrists, podiatrists, etc.) aged 40-75. The Nurses’ Health Study I was established in 1976 with 121,071 registered nurses, aged 30-55, in the 11 most populous US states. The Nurses’ Health Study II enrolled 116,429 female nurses in 1989, aged 25-42. All groups completed bi-annual questionnaires about demographics, lifestyle factors, medical history, and disease outcomes.
Patients: Men from Health Professionals Follow-Up Study and women from Nurses’ Health Study I and II with complete dietary intake measurement and no cancer diagnosis at baseline.
Interventions/Exposure: Assessment of ultra-processed food consumption using the Food Frequency Questionnaire (FFQ), which is a validated, semiquantitative instrument assessing intake of 130 food items and was administered to study participants every 4 years.
Using the NOVA classification, individual foods were classified as unprocessed or minimally processed, processed, or ultra-processed foods (Figure 1). Ultra-processed foods are generally defined as ready-to-eat or ready-to-heat formulations that contain little whole foods and commonly contain artificial sweeteners, food preservatives, and contaminants that migrate from the packaging.
Outcome: CRC, defined as proximal CRC if it occurred proximal to splenic flexure, distal CRC encompassing sigmoid and descending colon, and rectal encompassing rectum and recto-sigmoid junction. CRC diagnosis was confirmed by review of medical records and pathology reports.
Data Analysis: Hazard ratios (HR) calculated using Cox proportional hazards model after adjusting for age, sex, smoking, family history of cancer, history of endoscopy, physical activity, aspirin use, menopause status, and total caloric intake. Additional sensitivity analysis also accounted for body mass index (BMI) to differentiate impact of obesity from high ultra-processed food consumption. Based on FFQ data, individuals were categorized into 5 quintiles for ultra-processed food consumption with the lowest quintile used as the reference standard.
Funding: The National Institute of Health.
Results: Valid dietary data was available for 46,341 men (mean age 55, 91% White, mean BMI of 25, 10% current smokers) and 159,907 women (mean age 53, 98% White, mean BMI of 25, 21% current smokers) from the 3 cohorts. During 24-28 years of follow-up in the 3 cohorts, 1,294 cases of CRC were diagnosed in men and 1,922 cases were diagnosed in women.
In multivariate analysis, men who consumed the most ultra-processed foods (highest quintile or highest fifth) were 29% more likely to develop CRC compared to men who were in the lowest quintile (or lowest fifth): adjusted HR (aHR) 1.29 (95% confidence interval [CI] 1.08-1.53). When stratified by proximal vs distal CRC, this association was limited to distal CRC: aHR 1.72; 95% CI 1.24-2.37. Among sub-groups of ultra-processed foods, high intake of sugar-sweetened beverages (aHR 1.21; 95% CI 1.01-1.44) and high intake of ready-to-eat meat/poultry/fish products (aHR 1.44; 95% CI 1.20-1.73) was associated with an increased risk of CRC.
No overall association was identified between high consumption of ultra-processed foods and CRC in women, although high consumption of ready-to-eat/heat-mixed dishes was associated with an increased CRC risk in women: aHR 1.17; 95% CI 1.01-1.36.
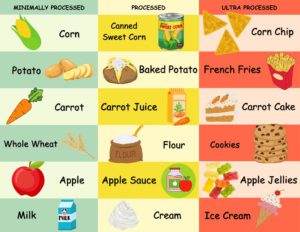 Figure 1. Processed food chart
Figure 1. Processed food chart
COMMENTARY
Why Is This Important?
Screening with colonoscopy and stool-based tests has led to significant decreases in CRC in the average-risk population. Still, when I speak briefly with patients after their colonoscopy, they frequently ask me if diet changes may minimize their risk of CRC. I usually emphasize that the most important intervention is to stay up to date with their CRC screening tests, but I note that eating more fresh fruits and vegetables and whole grains is beneficial,1 while intake of well-cooked red meat should be minimized. With this study, and other research2-3 based on the Nurses’ Health Study and Health Professionals Follow-Up Study, we can better educate patients that ultra-processed foods (e.g., ready-to-eat or ready-to-heat formulations that contain little whole foods and commonly contain artificial sweeteners, food preservatives, and contaminants that migrate from the packaging) should be avoided.
These types of data may be particularly helpful when addressing the rapid rise of CRC incidence in adults <50 years old,4 which is commonly defined as early-onset CRC. Excessive intake of sugar-sweetened beverages in adolescence and early adulthood as well as developing obesity in early adulthood are associated with an increased risk of early onset-CRC in women,2-3 while the use of GLP-1 receptor agonists,5 which have been incredibly effective at treating obesity and type II diabetes mellitus, has been associated with decreased risk of CRC. It seems likely that efforts to reduce early-onset CRC incidence will continue to explore diet interventions, lifestyle changes, and maintenance of a healthy BMI, as well as studying food additives that may have a pro-inflammatory impact on the gut microbiome or be carcinogens.
Key Study Findings
This finding was confirmed in sensitivity analysis after adjusting for obesity in the patient population, suggesting that high intake of ultra-processed foods was not simply a marker for obesity, which is a known risk factor for CRC.
Caution
Although the Nurses’ Health Study and the Health Professionals Follow-Up Study are among the best designed prospective cohort studies from the US, the vast majority of participants are White nurses and physicians, which limits generalizability. Also, although the Food Frequency Questionnaire is validated, it was only given to study participants every 4 years and may have limited accuracy to quantify intake of different foods.
My Practice
When my patients ask me what they can do to reduce their risk of CRC, the answers are rather straightforward. Get more aerobic exercise, eat a diet high in unprocessed or minimally processed foods with plenty of fresh fruits and vegetables, don’t smoke cigarettes, only drink alcohol occasionally, if at all, and maintain a healthy weight (i.e., don’t be obese or overweight based on BMI).1 Easier said than done! Nevertheless, these lifestyle factors minimize the risk of cancer, cardiovascular disease, and many other disorders.
This study provides excellent data to reinforce specific diet changes that may minimize the risk of CRC, independent of obesity or overweight status. Although the widespread availability of ultra-processed foods, including “junk foods” in convenience stores and “fast food” from chain restaurants, may be tempting, these foods should be consumed in moderation while emphasizing consumption of fresh fruits, vegetables, and whole grains.
For Future Research
Additional studies in women are needed to assess the interaction between menopause, hormonal changes, diet, and their impact on CRC risk. Also, more research into dietary risk factors, obesity, and other potential risk factors for early onset CRC need to be explored as well as the impact of dietary factors on CRC risk at specific anatomic sites.
Conflict of Interest
Dr. Schoenfeld reports no relevant conflicts of interest.
REFERENCES
- Centers for Disease Control and Prevention. What are the risk factors for colorectal cancer. www.cdc.gov/cancer/colorectal/basic_info Updated February 23, 2023. Accessed 1 March 2024.
- Liu PH, Wu K, Ng K, et al. Association of obesity with risk of early-onset colorectal cancer among women. JAMA Oncol 2019; 5: 37-44.
- Hur J, Otegbeye E, Joh HK, et al. Sugar-sweetened beverage intake in adulthood and adolescence and risk of early-onset colorectal cancer among women. Gut 2021; 70: 2330-36.
- Koh B, Tan DJH, Ng CH, et al. Patterns in cancer incidence among people Younger than 50 Years in the U, 2010 to 2019. JAMA Network Open 2023; 6: e2328171.
- Wang L, Wang W, Kaelber DC, et al. GLP-1 Receptor agonists and colorectal cancer risk in drug-naïve patients with type 2 diabetes, with and without overweight/obesity. JAMA Oncol 2024; 10: 256-58.

