The Long Road to Achieving Competence in Cold Snare Polypectomy: Video-Based Feedback Can Help

Swati G. Patel, MD, MS
Associate Professor of Medicine, University of Colorado Anschutz Medical Center; Rocky Mountain Regional Veterans Affairs Medical Center, Denver, Colorado
This summary reviews Kaltenbach T, Patel SG, Nguyen-Vu T, et al. Varied trainee competence in cold snare polypectomy – Results of the COMPLETE randomized controlled trial. Am J Gastroenterol. 2023 Jun 13. doi: 10.14309/ajg.0000000000002368. Online ahead of print.
Correspondence to Swati G. Patel, MD, MS. Associate Editor. Email: EBGI@gi.org
Access the article through PubMed
STRUCTURED ABSTRACT
Question: Does structured video-based feedback accelerate Gastroenterology trainee competence in cold snare polypectomy?
Study Design: Single-blinded randomized controlled trial where consecutive cold snare polypectomies performed by trainees were video recorded.
Setting: Two US academic medical centers 2017-2020.
Participants: Senior gastroenterology trainees (second- or third-year fellows) who had completed an average of 140 colonoscopies prior to the study.
Intervention: Video-based feedback on polypectomy technique every 2 weeks. Feedback used the ACT approach: 1) ask the trainee, 2) conversation between the trainee and the trainer, and 3) review the take home message. The videos included trainee’s videos and expert videos. Those randomized to the control group received conventional feedback at the discretion of their supervising ‘attending endoscopists.
Outcomes: Learning curve in achieving competence in cold snare polypectomy. Competence was assessed by a group of eight board certified gastroenterologists experienced in colon polyp resection. Each reviewer viewed the trainees’ polypectomy videos and scored them according to the cold snare polypectomy assessment tool, a validated 12-item competency assessment tool that includes an overall assessment.1 Competence was defined as a median score higher than 3 (4-perfect, 3-adequate, 2-sub-optimal, 1-unacceptable) on the overall assessment in the final 20 polypectomies a trainee performed.
Data Analysis: Learning curves were created using cumulative sum control curves at intervals of approximately 25 polyps. The sample size calculation was performed assuming that the video feedback group would achieve competency with 100 polypectomies +/-25 while the conventional feedback group would achieve competency with 150 polypectomies +/-25. This assumption required 8 trainees in each group.
Funding: American Society for Gastrointestinal Endoscopy Research Award.
Results: Twenty-two trainees participated (12 randomized to video feedback, 10 to conventional training) and completed 2,339 cold snare polypectomies. Only 2 trainees out of 12 (16.7%) in the video-feedback group achieved competence (after a mean of 135 polypectomies), whereas no trainees in the control group achieved competence (P=0.481). When extrapolating the association of cold snare polypectomy volume with performance, competence increased by 3% every 20 polypectomies in the video feedback arm, whereas there was no change in the control arm over polypectomy volume (Figure 1).
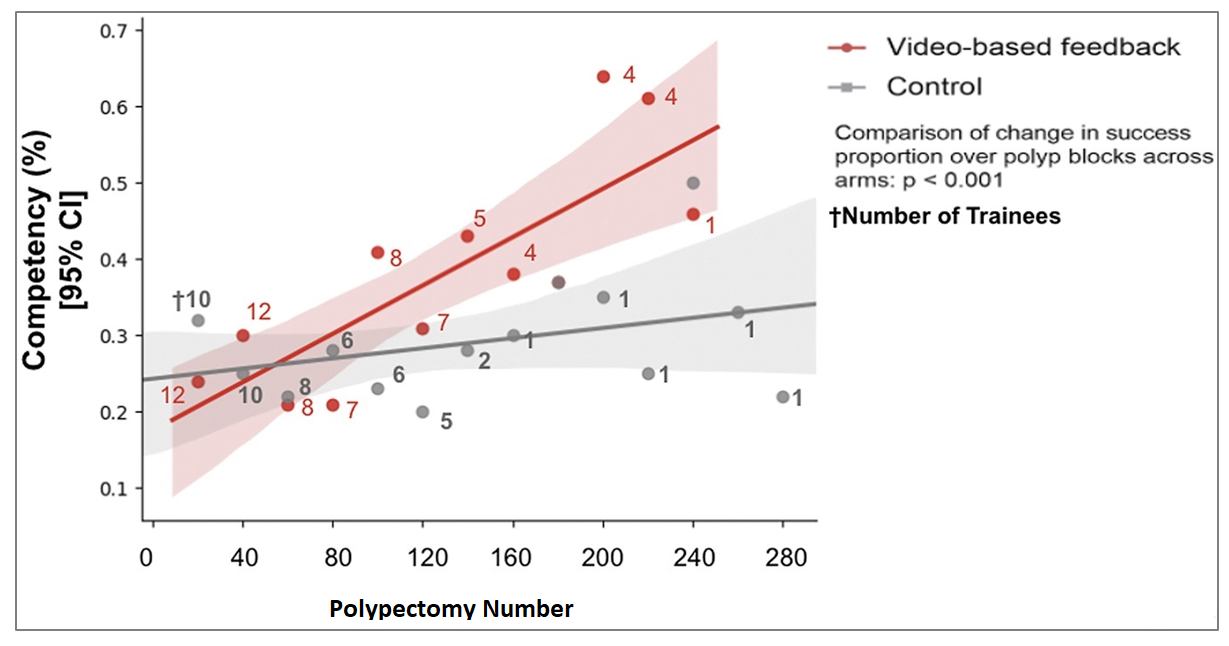
Figure 1. Change in success proportion of polypectomies among the video-based feedback group (red) and control group (gray). The trainees completed a variable amount of polypectomies during the study period, with approximately 1 trainee completing more than 280 polypectomies. † Represents the number of trainees used to calculate the success proportion for every 20 polypectomies.
COMMENTARY
Why Is This Important?
Colonoscopy and polyp removal are cornerstones of effective colorectal cancer screening and prevention.2, 3 Incomplete polyp removal is associated with a significantly increased risk of advanced colorectal neoplasia in the segment of the colon on surveillance colonoscopy4 (See March 2022 EBGI summary by Jeff Lee). Unfortunately, approximately 10%-20% of all post-colonoscopy colorectal cancers are due to incomplete resection of polyps,5 as reviewed by Dr. Jeffrey Lee in EBGI in March 2023. Small polyps (<10mm) are the most commonly found polyps during colonoscopy, and they can be removed safely, completely, and efficiently via cold snare polypectomy. Cold snare polypectomy is therefore a core skill for practicing gastroenterologists. There is little data on learning curves for this important skill among trainees and effective interventions to improve competence.
Key Study Findings
The majority of trainees in the study did not achieve competence, despite having baseline experience of 140 colonoscopies, and then completing an additional 56-58 colonoscopies as part of the study, wherein they completed an average of 106 cold snare polypectomies each. Two of the 12 trainees who received feedback achieved competence, whereas none of the trainees in the control arm did. Although there was no statistically significant difference in the proportion of trainees who achieved competence between the groups, providing trainees video-based feedback every two weeks resulted in a steeper learning curve than no feedback (Figure 1).
Caution
This study demonstrates that the learning curve for achieving competence in cold snare polypectomy is very slow. Although video-based feedback accelerates the learning curve, it seems impractical to implement video review of consecutive trainee cold snare polypectomies and trainer-trainee feedback sessions every two weeks. With that said, this model can be adapted by having trainees view a selection of their own videos, as well as expert videos. This approach would require further study to determine whether it has the same impact on learning curves.
My Practice
The bottom line is that cold snare polypectomy is an important skill that takes a very long time to master. I emphasize to the trainees in our program that they will likely not master this skill by the end of their fellowship and that they must dedicate intentional practice in this skill in the first years of independent practice. I encourage graduating fellows to ensure they join practices where they can receive peer guidance and feedback, not only in this important skill, but the many clinical and procedural skills that will continue to develop when one enters independent practice. I also encourage trainees to embrace humility about colorectal lesions they encounter, but may not be able to resect. It is always reasonable to mark the lesion with a tattoo and refer to a colleague. Although there is always the fear that patients will be frustrated with repeat procedures, when explained carefully that the ultimate goal is cancer prevention, patients will understand that quality of resection is of utmost importance.
For Future Research
This study shows that video-based feedback accelerates learning curves in cold snare polypectomy, however the learning curve is very slow with most trainees not achieving competence. Future work needs to be dedicated on how we can incorporate automated video-based feedback into training without taxing individual trainers.
Conflict of Interest
Dr. Patel was a co-author and investigator of this study.
@swatigp and @rkeshwanimd
REFERENCES
- Patel SG, Duloy AM, Kaltenbach T, et al. Development and validation of a video-based cold snare polypectomy assessment tool (CSPAT). Gastrointest Endosc 2019;89:1222-1230.
- Winawer SJ, Zauber AG, Ho MN, et al. Prevention of colorectal cancer by colonoscopic polypectomy. The National Polyp Study Workgroup. N Engl J Med 1993;329:1977-81.
- Zauber AG, Winawer SJ, O’Brien MJ, et al. Colonoscopic polypectomy and long-term prevention of colorectal-cancer deaths. N Engl J Med 2012;366:687-96.
- Pohl H, Anderson JC, Aguilera- Fish A, et al. Recurrence of colo rectal neo plastic polyps after in complete re section. Ann Intern Med 2021;174:1377-1384.
- Leung LJ, Lee JK, Merchant SA, et al. Post-colonoscopy colorectal cancer etiologies in a large inte grated US health care setting. Gastroenterol 2023;164:470- 472 e3.

