Cold Snare Decreases Post-Polypectomy Bleeding Vs Hot Snare for Small (≤10mm) Polyps

Philip Schoenfeld, MD, MSEd, MSc (Epi)
Chief (Emeritus), Gastroenterology Section, John D. Dingell VA Medical Center, Detroit, MI
Correspondence to Philip Schoenfeld, MD, MSEd, MSc (Epi), Editor-in-Chief. Email: EBGI@gi.org
This summary reviews Chang LC, Chang CY, Chen CY, et al. Cold versus hot snare polypectomy for small colorectal polyps: A pragmatic randomized controlled trial. Annals Intern Med 2023; In Press. doi: 10.7326/M22-2189.
Access the article through PubMed
STRUCTURED ABSTRACT
Question: Does cold snare polypectomy (CSP) decrease post-polypectomy bleeding compared to hot snare polypectomy (HSP) for small polyps (4-10 mm)?
Design: Multi-center, unblinded, randomized controlled trial (RCT) with concealed allocation and 1:1 randomization without stratification at the time small polyps were identified.
Setting: Six sites in Taiwan.
Patients: Inclusion criteria were: (a) individual >40 years old; (b) colonoscopy performed for screening or colon polyp surveillance, and (c) polyps 4-10 mm in diameter. Exclusion criteria included inadequate bowel preparation. Individuals who continued on antiplatelet or anticoagulant therapy during colonoscopy were also enrolled.
Interventions/Exposure: CSP vs HSP with electrocautery. Hemoclips could be placed post-polypectomy at discretion of the endoscopist if vessel was exposed or bleeding developed immediately postpolypectomy.
Outcome: The primary endpoint was delayed bleeding, which was defined as rectal bleeding within 14 days of leaving the endoscopy unit. Rectal bleeding with spontaneous cessation was defined as mild bleeding and severe delayed bleeding was defined as rectal bleeding with a decrease in hemoglobin of >20g/l, blood transfusion required, or repeat colonoscopic hemostasis. Multiple secondary outcomes were assessed including mean polypectomy time (measured from appearance of snare on the monitor to time endoscope was withdrawn from the lesion), mean procedure time, en bloc resection, and complete histologic resection. Each study participant was interviewed by phone at 2- and 14-days post-colonoscopy to assess study outcomes.
Data Analysis: Intention-to-treat analysis to assess superiority of CSP vs HSP to reduce delayed bleeding. Kaplan-Meier plots and log-rank test were used to assess differences in the primary outcomes. Generalized estimating equations with binomial distribution were used to explore impact of polypectomy technique on secondary outcomes. Planned risk factor analysis was not performed because there were so few bleeding events.
Funding: Partial funding from Boston Scientific Corporation, who had no role in study design, data analysis, or manuscript preparation.
Results: Overall, 4,270 individuals with small polyps were randomized (mean age: 62 years old; 60-61% male; colonoscopy complete to cecum: 99%; anticoagulant use: 2% with >75% discontinuing prior to colonoscopy; antiplatelet use: 11% with >85% discontinuing prior to colonoscopy). Post-polypectomy hemoclips were applied more frequently after HSP vs CSP (27.6% vs 18.9, P< 0.01). Delayed post-polypectomy bleeding (any type), mild bleeding characterized as rectal bleeding with spontaneous cessation, and severe delayed bleeding characterized by hemoglobin decrease of >20 g/l, need for blood transfusion, or need for repeat colonoscopy with hemostasis were all more frequent with HSP vs CSP (Table 1), although overall bleeding rates were low. Specifically, severe delayed bleeding only occurred in 1 patient in the CSP group (0.05%) and 8 patients (0.4%) in the HSP group. No differences in successful en bloc resection rates or complete histologic resection rates occurred, although mean polypectomy time and mean procedure time were both shorter with CSP vs HSP (Table 1).
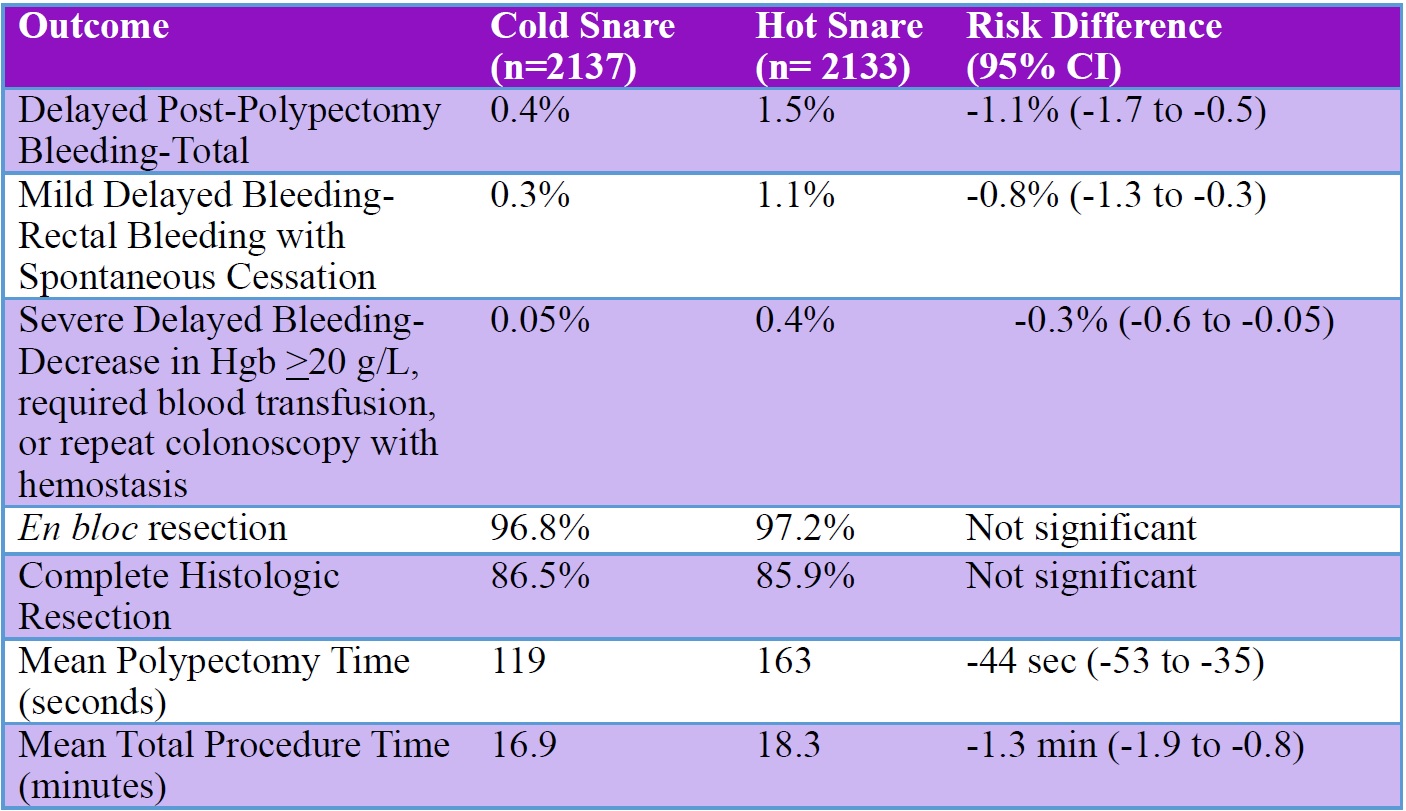
Table 1. Primary and secondary study outcomes. CI, confidence interval.
COMMENTARY
Why Is This Important?
CSP produces shallower resection depth in the submucosa compared to HSP where electrocautery may produce more severe and deeper submucosal injury, including in the muscularis propria, which could be expected to produce increased arterial damage and delayed post-polypectomy bleeding. However, no prior RCT has demonstrated a significant decrease in severe delayed post-polypectomy bleeding with CSP vs HSP, which is probably due to insufficient sample size since the rate of this adverse event is quite small.1 This well-designed RCT of over 4,000 patients with small adenomas finally confirms that CSP reduces this severe adverse event compared to HSP.
This is important since European guidelines2 do not strongly recommend CSP for small polyps. While US multi-society guidelines3 do strongly recommend CSP for small polyps, they also note wide variability in polypectomy practices in the US. Thus, this important RCT conducted by Dr. Li-Chun Chang and colleagues at 6 Taiwanese medical centers provides further support that CSP is not only as effective as HSP but also is safer too! Our goal moving forward should be to educate and advocate for endoscopists to minimize use of HSP for small polyps while eliminating use of hot biopsy forceps, which is inefficient as well as associated with deep tissue injury.
Key Study Findings Severe delayed post-polypectomy bleeding was more frequent after HSP vs CSP (0.4% vs 0.05%; risk difference: -0.3%; 95% confidence interval [CI]: -0.6% to -0.05%) while CSP produced shorter mean polypectomy time (risk difference: -44 seconds; 95% CI: -53 to -35) and shorter total procedure time (16.9 minutes vs 18.3 minutes; risk difference: -1.3 minutes; 95% CI: -1.9 to -0.8).
Caution
The post-polypectomy bleeding rates were quite low in this study and may reflect the liberal use of hemoclips after polypectomy, which was significantly greater with HSP vs CSP (27.6% vs 18.9%, P< 0.01). The frequent use of hemoclips after HSP probably decreased post-polypectomy bleeding in this group and minimized the difference vs CSP. Although it is impossible to blind endoscopists to use of CSP vs HSP, it seems that endoscopist knowledge that they were performing HSP may have disproportionately increased their use with HSP. Nevertheless, using hemoclips in >25% of small polyp resections would not be standard of care in the US.
My Practice
Per the US Multi-Society Task Force on Colorectal Cancer Recommendations on Endoscopic Removal of Colorectal Lesions3, I routinely perform CSP on all polyps <10 mm because it’s faster than performing HSP. Although indirect evidence suggested that CSP would reduce severe delayed post-polypectomy bleeding, this RCT confirms this, which confirms the importance of emphasizing CSP. I never use hot biopsy forceps, although I’m anecdotally aware of surgical colleagues who continue to use this. I generally reserve HSP for pedunculated polyps > 10 mm, although I use CSP for piecemeal polypectomy of large sessile polyps.4
When using CSP for polyps 4-10 mm, I strive to obtain a 2 mm margin of normal colonic mucosa at the resection site to ensure complete resection and should produce the sunny side egg up appearance.5 I also use jumbo forceps to remove tiny polyps 1-3 mm depending on the position of the polyp in the colon. 6
For Future Research
Larger studies about the safety of CSP among high-risk patients who cannot discontinue antiplatelet or anticoagulants may be helpful. However, research to identify endoscopists with high-volume of HSP (or even hot biopsy forceps resection) followed by implementation research to increase CSP use could be more beneficial for our patients.
Conflict of Interest
Dr. Schoenfeld reports no conflicts of interest.
REFERENCES
- de Benito Sanz M, Hernandes L, Garcia Martinez MI, et al. Efficacy and safety of cold versus hot snare polypectomy for small (5-9 mm) colorectal polyps: a multicenter randomized controlled trial. Endoscopy 2022; 54: 35-44.
- Ferlitsch M, Moss A, Hassan C, et al. Colorectal polypectomy and endoscopic mucosal resection (EMPR): European Society of Gastrointestinal Endoscopy clinical guideline. Endoscopy 2017; 49: 270-297.
- Kaltenbach T, Anderson JC, Burke CA, et l. Endoscopic removal of colorectal lesions-recommendations by the US Multi-Society Task Force on Colorectal Cancer. Gastrointest Endosc 2020: 91: 486-519.
- Lee J. Increased risk of metachronous neoplasia after incomplete polyp resection—time to CARE about polypectomy technique. Evidence-Based GI March 2, 2022. https://gi.org/journals-publications/ebgi/lee_february2022/. Accessed March 9, 2023.
- Patel S. Piecemeal cold snare polypectomy of large sessile serrated polyps is safe and effective: cold is the new hot! Evidence-Based GI October 22, 2021. https://gi.org/journals-publications/ebgi/piecemeal-cold-snare-polypectomy-of-large-ssp-cold-is-the-new-hot/. Accessed March 9, 2023.
- Kumar S. Tiny polyps—it’s OK to remove polyps <3 mm with large or jumbo biopsy forceps. Evidence-Based GI August 11, 2022. https://gi.org/journals-publications/ebgi/kumar_august_2022/. Accessed March 9, 2023.
Download the Article Summary (PDF)
Download the Article Summary (PDF)

